 三甲
三甲
股骨头坏死的病因学/病理生理学机制研究进展:2021年
股骨头坏死的病因学/病理生理学机制研究进展:2021年
作者:P Guggenbuhl, F Robin, S Cadiou, J D Albert
作者单位: Université de Rennes, INSERM, CHU Rennes, institut NUMECAN (Nutrition Metabolisms and Cancer), UMR 1241, 35000 Rennes, France. Electronic address: pascal.guggenbuhl@chu-rennes.fr.
译者:陶可(北京大学人民医院骨关节科)
摘要
股骨头(ONFH)缺血性骨坏死是临床医生需要了解的髋关节疼痛的原因之一。在许多情况下,出于其他原因进行骨盆X线拍照时,偶然发现了股骨头坏死ONFH。在其他情况下,疼痛提示可能存在股骨头坏死ONFH。对于风湿病学家(骨科医生)而言,工作的主要部分是寻找原因。在大约70%的股骨头坏死ONFH病例中,可以明确病因。其中一些是显而易见的,背景可以诊断(皮质类固醇激素,酗酒……)。但是,在许多情况下,需要进行其他的影像学检查以进行病因诊断。在某些情况下,针对病因治疗可以防止股骨头坏死ONFH的复发。
关键词:酒精;缺血性骨坏死;股骨头缺血性骨坏死;皮质类固醇;骨坏死。
介绍
股骨头(ONFH)缺血性骨坏死是临床医生需要了解的髋关节疼痛的原因之一。在许多情况下,出于其他原因进行骨盆X线拍照时,偶然发现了股骨头坏死ONFH。在其他情况下,疼痛提示可能存在股骨头坏死ONFH。髋关节疼痛最常见于腹股沟区和大腿前方,用力或髋关节位置变动后髋关节疼痛突然出现。最初疼痛可能很强烈,伴随有炎症性夜间觉醒的痛感。然而,通常情况下,疼痛会迅速变成机械性的,表现为当患者将足部放在地板上,而当负重解除或限制髋关节活动幅度时(尤其是内旋),疼痛得以消失。这是对所有髋关节疾病的鉴别诊断,尤其是关节炎或骨关节炎,以及其他骨骼系统疾病。本文及所有影像学检查(在本期的另一章中)有助于获得诊断。
对于风湿病学家而言,工作的主要部分是寻找原因,在某些患者中,这是发现未知疾病的机会。对于其他人来说,这是一种已知的疾病的并发症。
在本文中,我们将着重回顾一下最主要原因的常见部分以及针对病因治疗的可考虑因素。
术语“缺血性”骨坏死表明生理血管形成的中断。股骨头血供系统是终末循环,就像在心脏或大脑中,动脉阻塞或中断会导致器官坏死,在这种情况下,会发生股骨头骨坏死[1]。然而,股骨头坏死ONFH生理病理学更为复杂,公认的股骨头坏死ONFH是血管损害与骨细胞的改变,尤其是这些骨细胞是机械感知细胞和一些尚未阐明的遗传因素之间的相互作用的结果[2]。
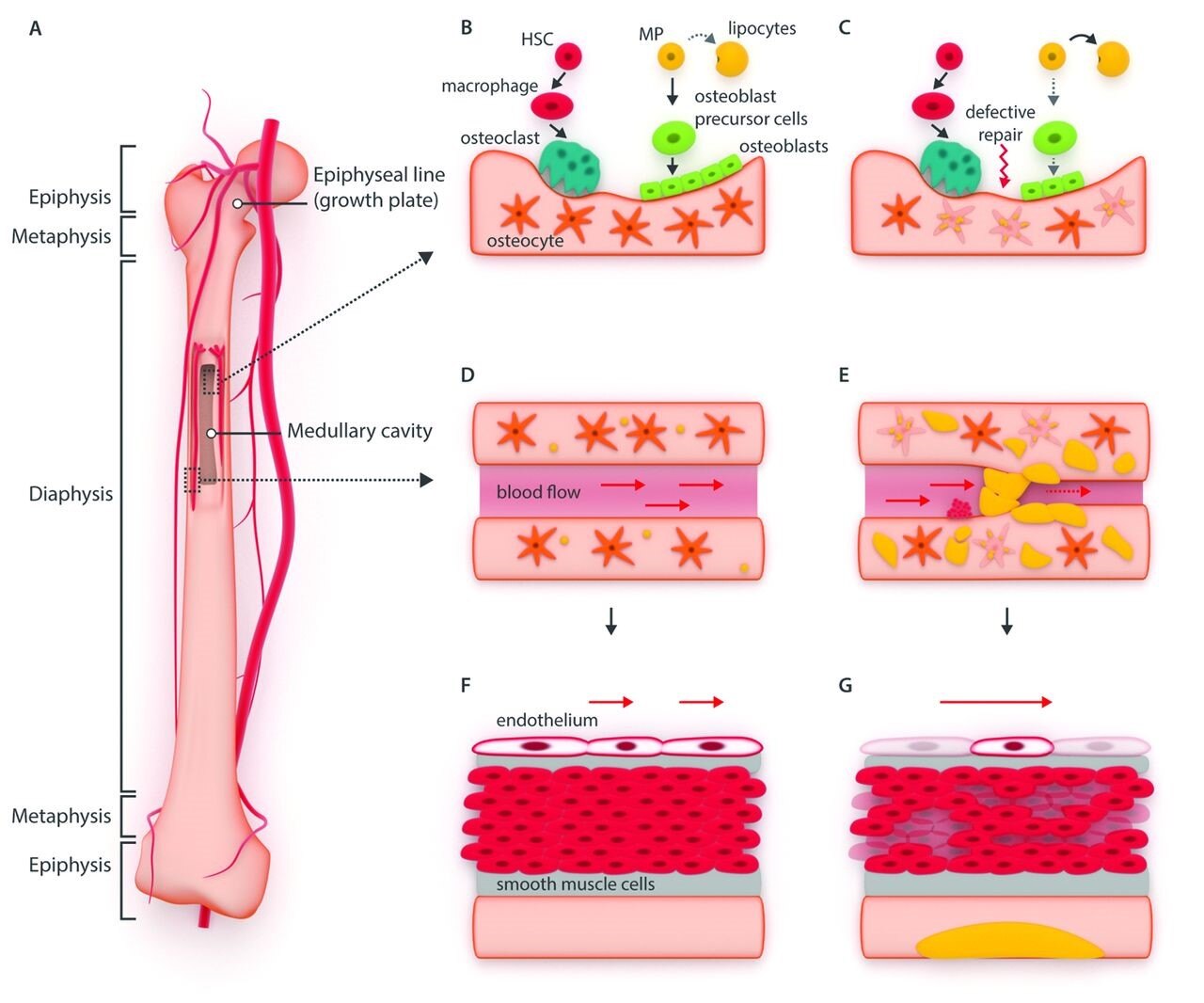
两种机制可以导致股骨头坏死ONFH:创伤,包括局部或系统性原因。在第一种情况下,缺血通常继发于巨大创伤(如骨折或完全的股骨头血管系统的破坏)。有时,也可能继发于较小的创伤。在第二种情况下,血管病变可能来自病理性血管内阻塞物(脂质体或气态微栓塞;高凝状态),血管外压力(骨髓脂肪细胞肥大,骨髓水肿,骨髓异常增殖症)或骨质破坏(骨细胞损伤)(酒精或药物细胞毒性反应)[3]。股骨头是骨坏死最常见位置。这可能是由于其特定的血管构成。大多数股骨头血液供应来源于股骨头上外侧负重区域的滋养管动脉[2][4]。
股骨头坏死的危险因素
临床医生必须检查危险因素,尤其是那些可以改进或处理的危险因素。必须说,许多机制都是所有原因共同的原因,最常见的往往又是复杂的。在少数情况下,不是很好估计(约15%至30%)原因不明,也无法查找原因[3][5][6](图1)。
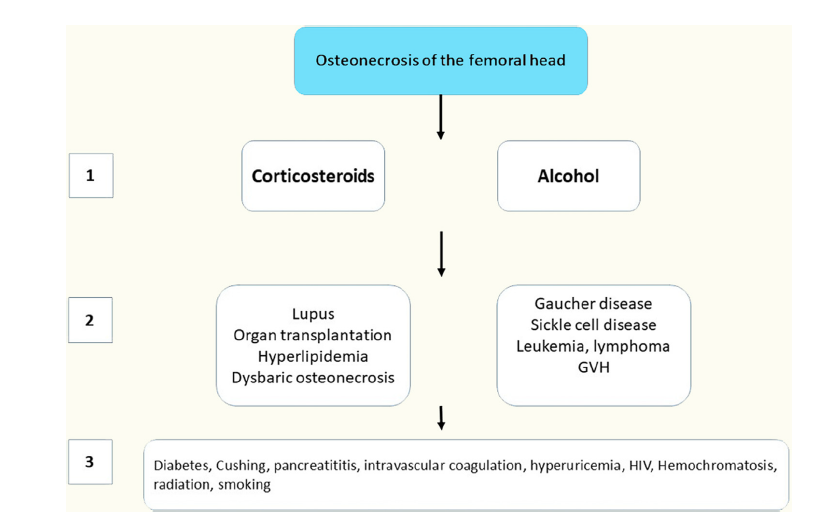
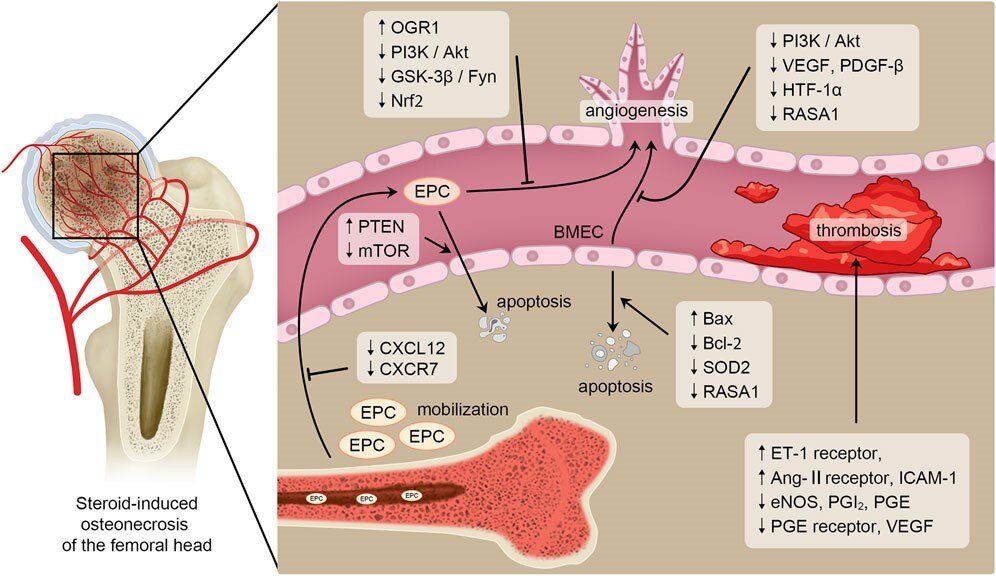
Figure 1 Progressive diagnosis diagram to determine the main causes of osteonecrosis of the femoral head from the most frequent causes (1) to the rarest causes (3).
图1 渐进式诊断图确定了股骨头坏死的主要原因,从最常见原因(1)到最罕见原因(3)。
Osteonecrosis in children with acute lymphoblastic leukemia | Haematologica
儿童急性淋巴细胞白血病的骨坏死| 血液学
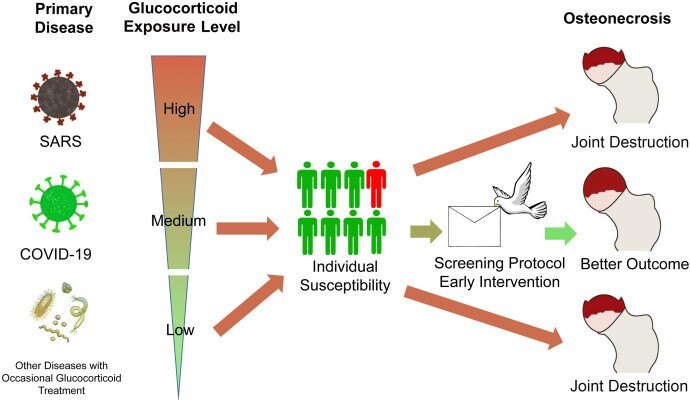
General recommendation for assessment and management on the risk of glucocorticoid-induced osteonecrosis in patients with COVID-19
评估和管理新冠COVID-19患者糖皮质激素诱导的股骨头坏死风险的一般建议
最常见的风险因素
在超过80%的病例中,(皮质类固醇)激素和酒精是主要原因[7]。
皮质类固醇激素
这是非创伤性股骨头坏死ONFH的最常见原因。在一项纳入3000例非创伤性股骨头坏死病例中,在30%的病例曾使用过激素,其次是20%的患者曾有酒精摄入。在系统性红斑狼疮(SLE)的情况下,激素似乎更有害,这是股骨头坏死ONFH的另一个潜在原因[8]。而且风险随着剂量增加和治疗持续时间的增加而增加,且无法在文献中找到阈值(即最小的可能导致股骨头坏死的剂量)。在包括23561例患者在内的57项研究meta分析中,Mont等人发现,如果激素治疗超过2 g泼尼松等效剂量时,股骨头坏死ONFH发病率为6.7%,且每10 mg/d增加发病率3.6%。高于20 mg/d的阈值增加了风险,而<15 mg/d,则阈值相对较低[9]。即使以相对较低剂量的短期治疗也会增加股骨头坏死的风险。Dilisio在一个非常大的美国病例队列中发现,与未接受激素治疗的患者相比,接受了超过6天、每天4mg(一盒21片)甲泼尼松龙片的患者的股骨头坏死风险增加了1.6倍[10]。
已经有许多机制来解释激素导致股骨头坏死ONFH的发生原因。①在骨重塑水平上,已经描述了骨细胞凋亡和/或成骨细胞自噬的增加。②与酒精毒性情况下相似,脂肪细胞的分化增加从而导致成骨细胞分化的剥夺。这会引起脂肪细胞数量和体积的增加,从而导致骨组织压力升高、骨膜间微循环破坏和股骨头骨结构变化。③激素会诱导血管内皮细胞损伤和复杂的凝血病变,引发血栓形成。④微生物组学,氧化应激,遗传和表观遗传和mi-RNA也有潜在的作用,该作用将间充质干细胞向成脂肪细胞分化而非成骨祖细胞分化。⑤最后,从Kenzora和Glimcher[11]出现了“多次打击假说”的概念,这表明单一机制不足以诱导股骨头坏死。例如,激素诱导的股骨头坏死患者在SLE病例中比健康患者或其他病理状况的患者更常见[8]。
滥用酒精/酗酒
过度使用酒精已与约20-30%患有股骨头坏死患者有关。相较于激素诱发的股骨头坏死ONFH,已经提出了几种机制,例如骨形成减少,骨细胞凋亡或过量的脂质沉积,酒精所致的股骨头坏死也存在类似情况。最近有研究表明,在酒精诱导的股骨头的骨坏死中,mi-RNA具有异常表达,骨或血管基因靶标(包括IGF2,PDGFA,RUNX2,PTEN,PTEN,PTEN和VEGF)可能会异常表达。这些观察结果可能具有生理病理学和诊断价值[12]。
其他经典风险因素
Gaucher病
Gaucher病是股骨头坏死ONFH的经典病因,通常在多发性骨坏死病例中。这是由于溶酶体酶(β-葡萄糖神经酰胺酶)的缺乏,导致葡萄糖神经酰胺在单核巨噬细胞的溶酶体中蓄积,主要发生在肝脏、脾脏和骨髓中。骨关节表现通常最早,并导致主要出现Gaucher病相关的发病率和残疾率[13][14]。
系统性红斑狼疮SLE
在3-30%的SLE病例中会发生股骨头坏死[15],如前所述,激素似乎是主要危险因素。然而,SLE病例对激素诱导的股骨头坏死的敏感性似乎比其他疾病强[8]。最近,已经提出了NOS3,COL2A1和CR2基因中某些单核苷酸变异(SNV)的遗传倾向,分别参与骨骼或软骨形成,以及自身免疫性中的CR2基因表达[16]。
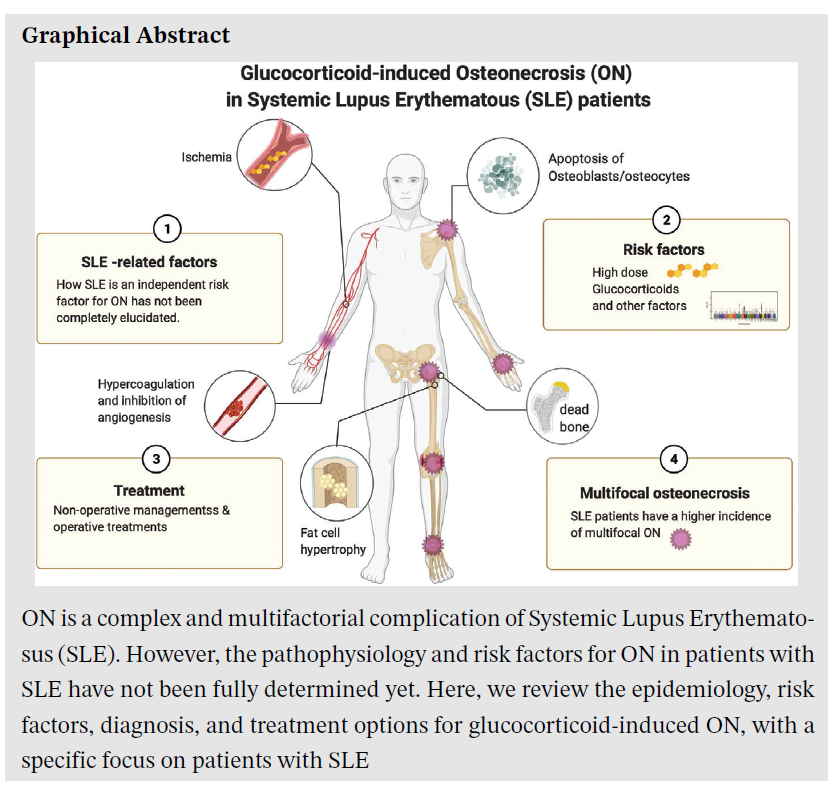
股骨头坏死是系统性红斑狼疮(SLE)的复杂且多因素并发症。然而,SLE患者发生股骨头坏死的病理生理学和危险因素尚未完全确定。在这里,我们回顾了糖皮质激素诱导股骨头坏死的流行病学、危险因素、诊断和治疗方案,特别关注SLE患者。
减压病性股骨头坏死(caisson病)[17]
这是另一个非常经典但罕见的股骨头坏死ONFH病因,在海底潜水员和工人呼吸压缩空气或气体之外。最公认的理论是,这是由于亚临床减压疾病(DCS)的长期表现。减压导致血液中的气体不能溶解而在骨微循环中形成气泡和栓塞,并激活凝血途径。结果导致骨组织内压力和股骨头坏死增加。股骨和胫骨骨干的骨坏死时有发生,有时会在行走负荷下出现疼痛,有时疼痛会非常强烈,骨折的危险很大。
器官移植和慢性肾衰竭/血液透析
器官移植中股骨头坏死ONFH的患病率估计在3%至41%之间。肾移植患者的研究最多。大多数研究都是回顾性的,具有不同的激素和免疫抑制疗法方案和影像学检查方式。在一项前瞻性研究中,在11%髋关节中存在股骨头坏死[18]。在肾移植后的2周内,患者接受的激素总剂量与股骨头坏死的发生有关[19]。在最近的一项回顾性研究中,肾脏移植受体中股骨头坏死ONFH的发病率降低(移植后十年时为4.1%)归因于过去十年中他克莫司替代环孢素。男性患者是股骨头坏死的独立危险因素。窃取性缺血综合征的假说认为由于同种异体移植肾脏导致了同种异体移植侧的早期股骨头坏死[20]。在现代肾移植管理中,激素剂量的降低也可能与肾脏移植受体的股骨头坏死ONFH减少有关。
高脂血症
高脂血症是股骨头坏死的经典原因。但是,很少有研究解决了这一主题。在112例患有急性淋巴细胞白血病的患者(儿童和年轻人)中,有22例出现症状性股骨头坏死。在这一人群中,高脂血症主要是甘油三酸酯和胆固醇水平升高与股骨头坏死风险增加有关。较高的HDL胆固醇和股骨头坏死之间存在反比关系的趋势。但是,LDL胆固醇与股骨头坏死无关[21]。高血清甘油三酸酯水平似乎也是系统性红斑狼疮中股骨头坏死ONFH的危险因素[22]。
血液学障碍
镰状细胞性贫血症
这篇评论的一章专门针对该病因。由于与红细胞形态有关的血管内阻塞,因此在这种情况下会经常出现股骨头坏死ONFH。临床化验通常有助于诊断。
白血病和淋巴瘤
在急性淋巴细胞白血病,、性髓样白血病和急性髓样淋巴瘤中,股骨头坏死的风险增加。激素似乎是主要的危险因素[15][23]。高剂量的激素是主要原因。股骨头坏死也是成人和儿童中骨髓移植和移植物抗宿主反应的并发症。移植后3年估计股骨头坏死发生率在6%至19%之间。激素和免疫抑制剂是主要危险因素[24]。
少见原因[3]
在较少见的病例中已经描述或发表了许多其他原因,可能与以前描述的股骨头坏死机制有关:糖尿病[25],库欣Cushing病[26],胰腺炎,血管内凝血[1],高尿素/痛风,HIV[27],血色素沉着症[28],辐射病[29],吸烟等。
结论
在大多数情况下可以找到股骨头坏死的原因。其中一些是显而易见的,背景可以诊断(激素,酗酒……)。但是,在许多情况下,需要进行影像学检查以进行病因诊断。我们提出了一种从最常见原因开始的诊断方法。关节外症状和病史应重点考虑(图1)。在某些情况下,病因的治疗可以防止疾病复发。
Introduction
Avascular osteonecrosis of the femoral head (ONFH) is one of the causes of hip pain that clinicians need to know about. In many cases, it is a fortuitous discovery when pelvic X-rays is performed for another reason. In the other cases, it is pain that reveals the disease. Hip pain is most commonly pain felt in the groin and anterior thigh, of sudden appearance after an effort or a change of position. Pain can be initially strong with nocturnal awakenings mimicking an inflammatory pain. However, rapidly and typically, the pain become mechanical, occurs when the patient put his foot on the floor and disappear in discharge with a functional impotence and variable joint limitation amplitudes, notably internal rotation. It is a differential diagnosis of all hip diseases, especially arthritis or osteoarthritis but also bone diseases. The context, and above all imaging (which is covered in another chapter of this issue) make the diagnosis.
For the rheumatologist, a major part of the job is to look for a cause and in some patients, it is the opportunity to discover an unknown disease. For others it is a complication of an already known disease.
In this paper, we will review the main causes of ONFH emphasizing the most frequent ones and those for which an etiological treatment can be considered.
The term “avascular” osteonecrosis suggests an interruption of the physiological vascularization. The femoral head vasculature is a terminal one and as in heart or brain, an arterial obstruction or interruption leads to organ necrosis, in this case osteonecrosis [1]. However, ONFH physiopathology is more complex and it is admitted that it is the result of an interaction between vessels damages, alteration of bone cells, especially osteocytes which are mechanosensory cells and some non-well-known genetic factors [2].
Two kinds of mechanisms can result in ONFH: traumatisms, which constitute local causes or systemic conditions. In the first case, ischemia is secondary to generally a huge traumatism followed by a fracture or a luxation and vasculature damages. It can be sometimes secondary to micro traumatisms. In the second case, the vascular lesions can come from pathologic intravascular obstruction (lipids or gaseous microemboli; hypercoagulability state), extravascular compression (medullary adipocytes hypertrophy, intra-medullary edema, intra-medullary proliferation) or bone damages especially of osteocytes (drugs or alcohol cytotoxicity) [3]. Femoral head is the more frequent location of osteonecrosis. It may be due to its particular vascularization. The majority of the blood supply originates from the retinacula arteries supplying the superolateral weight-bearing portion of the femoral head [2], [4].
Avascular osteonecrosis of the femoral head risk factors
Clinicians have to check for risk factors, especially those, few, which can be modified or treated. It must be said that many mechanisms are common to all causes, most often intricate. In a few cases, not very well estimated (approximately 15 to 30%), no cause is identified and no cause is found [3], [5], [6] (Fig. 1).
The most frequents risk factors
Corticosteroids and alcohol are the causal agents in more than 80% of the cases [7].
Corticosteroids
This is the most frequent cause of non-traumatic ONFH. In a series of 3000 cases of non-traumatic osteonecrosis, corticosteroids were in question in 30% of the cases, followed by alcohol, in 20%. Corticosteroids seemed to be more deleterious in case of systemic lupus erythematosus (SLE), another potential cause of ONFH [8]. If the risk increases with the increasing doses and the treatment duration, it is not possible to found thresholds in the literature. In a meta-analysis of Fifty-seven studies including 23,561 patients, Mont et al found that ONFH incidence was 6.7% if corticosteroid treatment exceeded 2 g prednisone-equivalent with a 3.6% increase with each 10 mg/d increase. A threshold superior to 20 mg/d increased the risk, which was lower if < 15 mg/d [9]. Even short periods of treatment with relatively low doses increase the risk. Dilisio found in a huge US cohort that patients who received one 21-tablet, 4-mg methylprednisolone taper pack taken over 6 days had an increased risk of 1.6 compared to patients who did not had this treatment [10].
Many mechanisms have been evoked to explain the occurrence of a steroid induced ONFH. At the bone remodeling level, osteocytes apoptosis and/or increase of osteoblast autophagy have been described. Adipocytes differentiation increase at the detriment of osteoblasts differentiation, which is similar in case of alcohol toxicity. This increase of adipocytes number and size with intracellular accumulation of lipids cause an increase in bone pressure and disruption in interosseous microcirculation and bone structural changes in the femoral head. Steroids induce vascular endothelial cells damages and a complex coagulopathy leading to vessels thrombosis. There is also a potential role for the microbiome, oxidative stress, genetic and epigenetic and mi-RNAs, which regulate the differentiation of mesenchymal stem cells into adipogenic or osteogenic progenitor cells. Finally the concept of “multi-hit hypothesis” as emerged from Kenzora and Glimcher [11], suggesting that a single mechanism is not sufficient to induce osteonecrosis; for example corticosteroids induced ONFH is more frequent in patients with SLE than in healthy people or patients with other pathological conditions [8].
Alcohol abuse
Overuse of alcohol has been associated to approximatively 20-30% of the patients who developed a hip osteonecrosis. As for steroid induced ONFH, several mechanisms have been suggested such as decreased bone formation, osteocyte apoptosis or excess lipid deposition; many of them seem likely to be shared. In an original way, it has recently be described that mi-RNAS could be aberrantly expressed in alcohol-induced osteonecrosis of femoral head, with bone or vessel genes targets including IGF2, PDGFA, RUNX2, PTEN, and VEGF. These observations could be of physiopathological and diagnosis interest [12].
The other classic risk factors
Gaucher disease
Gaucher disease is a classic etiology of ONFH, very often in a context of multiple osteonecrosis. It is due to a deficiency in the lysosomal enzyme β-glucocerebrosidase, which leads to accumulation of gluco-cerebroside in the lysosomes of mononuclear phagocytes, predominantly in the liver, spleen, and bone marrow. Osteoarticular manifestations are often inaugural and contribute significantly to the morbidity and disability associated with Gaucher disease [13], [14].
Systemic lupus erythematosus
Osteonecrosis in Lupus has been reported in 3-30% of the cases [15] and as said before, corticosteroids seemed to be a major risk factor. However, the susceptibility to steroids induced osteonecrosis seems to be stronger than for other diseases [8]. Very recently a genetic predisposition has been suggested with some Single Nucleotide Variations (SNVs) in NOS3, COL2A1, and CR2 genes, respectively involved in bone or cartilage formation and for CR2 in autoimmunity [16].
Dysbaric osteonecrosis (caisson disease) [17]
It is another very classic, but rare etiology of ONFH, outside of undersea divers and workers breathing compressed air or gas. The most accepted theory is that it is due to a long-term manifestation of sub-clinical decompression sickness (DCS). Decompression lead to dissolution of gas in blood with gas bubble formation and emboli in bone microcirculation with activation of coagulation process. The consequence is an increase in intraosseous pressure and osteonecrosis. Diaphysis osteonecrosis of the femur and the tibia can occur sometimes, with pain under load, sometimes very intense with a significant risk of fracture.
Organ transplantation and chronic renal failure/hemodialysis
The prevalence of ONFH in organs transplantation has been estimated between 3 to 41%. Patients with renal transplant have been the most studied. Most of the studies are retrospective, with different steroids and immunosuppressive therapies regimen and imaging modalities. In a prospective study, the incidence was lower with an osteonecrosis of the femoral head in 11% of the hips [18]. The total dose of steroid received by the patients in the 2 weeks following renal transplantation is related to osteonecrosis development [19]. In a recent retrospective study, the decrease of the incidence of ONFH in kidney transplant recipients (4.1% at ten years after the transplantation) was attributed to the replacement of cyclosporine by tacrolimus over the last decade. Males were independently associated to osteonecrosis. The hypothesis of an ischemic steal syndrome due to the allograft kidney leading to an early osteonecrosis at the allograft side has been proposed [20]. It is probable that the decrease of steroids doses in the modern management of kidney transplantation is also implicated in the decrease of ONFH in kidney transplant recipients.
Hyperlipidemia
Hyperlipidemia is a classic cause of osteonecrosis. However, few studies have addressed this topic. In 112 patients (children and young adults) with acute lymphoblastic leukemia, 22 experienced symptomatic osteonecrosis. In this population, hyperlipidemia was associated with an increased risk of developing osteonecrosis with increased triglycerides and cholesterol levels. There was a tendency of an inverse relationship between higher HDL cholesterol and osteonecrosis. However, prolonged increase of LDL cholesterol was not associated with osteonecrosis [21]. High serum triglyceride level seems also to be a risk factor for ONFH in systemic lupus erythematosus [22].
Hematological disorders
Sickle cell disease
A chapter of this review is specifically dedicated to this etiology. The ONFH is frequent in this context due to the intravascular obstruction linked to the red globules shape. The clinical context generally help in the diagnosis.
Leukemia and lymphoma
In acute lymphoblastic leukemia, chronic myeloid leukemia and acute myeloid lymphoma there is an increased risk of osteonecrosis. Steroids seems to be the major risk factor [15], [23]. High doses of corticosteroids are the main explanation. Osteonecrosis is also a complication of bone marrow transplantation and graft versus host reaction in adults and children. The frequency has been estimated between 6% and 19%, 3 years after transplantation. ONFH is the most common localization. Steroids and immunosuppressants are the major risk factors [24].
Less frequently [3]
A great number of other causes have been described or published in smaller series, potentially related to osteonecrosis mechanisms described before: diabetes [25], Cushing disease [26], pancreatitis, intravascular coagulation [1], hyperuricemia/gout, HIV [27], hemochromatosis [28], radiation [29], smoking…
Conclusion
A cause to ONFH can be found in a large number of cases. Some of them are evident and the context give the diagnosis (corticosteroids, alcohol abuse…). However, in many cases, additional tests to imaging are required to make the causal diagnosis. We propose a pragmatic approach beginning by the most frequent causes. Extra-articular symptoms and anamnesis are very important to consider (Fig. 1). In some cases, the treatment of the cause can prevent the recurrence of the disease.
Etiology of avascular osteonecrosis of the femoral head
Abstract
Avascular osteonecrosis of the femoral head (ONFH) is one of the causes of hip pain that clinicians need to know about. In many cases, it is a fortuitous discovery when pelvic X-rays is performed for another reason. In the other cases, pain reveals the disease. For the rheumatologist, a major part of the job is to look for a cause. An etiology can be found to ONFH in about 70% of the cases. Some of them are evident and the context give the diagnosis (corticosteroids, alcohol abuse…). However, in many cases, additional tests to imaging are required to make the causal diagnosis. In some cases, the treatment of the cause can prevent the recurrence of the disease.
Keywords: Alcohol; Avascular osteonecrosis; Avascular osteonecrosis of the femoral head; Corticosteroids; Osteonecrosis.
文献出处:P Guggenbuhl, F Robin, S Cadiou, J D Albert. Etiology of avascular osteonecrosis of the femoral head. Review Morphologie. 2021 Jun;105(349):80-84. doi: 10.1016/j.morpho.2020.12.002. Epub 2021 Jan 12.
本文是陶可版权所有,未经授权请勿转载。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论