 三甲
三甲
股骨头坏死保髋/保头治疗:股骨近端截骨术治疗股骨头缺血性坏死
文章摘要:通过将股骨头坏死区转移出主要负重区,将健康骨转移至负重区,从而延缓股骨头坏死的进展,促进坏死骨愈合。
股骨头坏死保髋/保头治疗:股骨近端截骨术治疗股骨头缺血性坏死
作者:Thorsten M Seyler, David R Marker, Slif D Ulrich, Tobias Fatscher, Michael A Mont
作者单位: Department for Orthopedic Surgery, University Hospital Berne, Freiburgstraße 8, 3010, Bern, Switzerland. christianesylvia.leibold@insel.ch.
译者:陶可(北京大学人民医院骨关节科)
摘要
目的:通过将股骨头坏死区转移出主要负重区,将健康骨转移至负重区,从而延缓股骨头坏死的进展,促进坏死骨愈合。
适应症:相对年轻的患者(年龄 < 50 岁)的局灶性股骨头骨坏死,无晚期退行性指征(Tönnis 等级 ≤ 1)。
禁忌症:X线显示髋关节退变(> Tönnis 1 级);广泛的缺血性坏死(Kerboul角 > 240°);晚期病变(≥骨循环研究协会[ARCO]分分期3b期)。
手术技术:通过进行髋关节脱位手术,可以完全暴露髋关节。股骨内翻截骨术用于将股骨头的坏死病变转出中央承重区并更靠近内侧。使用角稳定螺钉或钢板进行截骨处固定。通过活板门手术,可以从大转子直接清创(股骨头坏死骨)和自体骨移植。尽可能保留软骨瓣或用自体基质诱导软骨形成(AMIC)代替进行修复。
术后管理:住院期间,术后立即进行被动运动锻炼,以防止髋关节囊粘连。手术后,患者需要借助拐杖进行至少8周的15公斤的部分负重活动。限制用力外展、内收及屈曲90°以上,以保护大转子截骨(避免截骨处不愈合风险)。在8周随访时影像学确认截骨处愈合后,允许逐步恢复完全负重并开始外展肌训练。
结果:9例(10髋)股骨头坏死患者采用髋关节外科脱位内翻截骨术治疗。6髋采用自体植骨,4髋采用顺行钻孔(髓心减压)。4例缝合软骨损伤,2例需要AMIC治疗。手术时的平均年龄为29 ± 9岁(20-49岁),所有患者的平均随访时间为3 ± 2年(1-7年)。1例髋关节病情进展,随后进行全髋关节置换术。其他9个髋关节没有出现股骨头坏死进展,临床结果也有所改善。并发症为股骨截骨处假关节和大转子假关节形成。
关键词:髋关节脱位;骨坏死;截骨术;活板门手术;负重
手术原则和目的
股骨近端截骨术治疗股骨头坏死(ONFH)的目的是将坏死区域移出负重区域,从而延缓骨坏死进展甚至愈合。治疗股骨头坏死(ONFH)的股骨截骨术可分为成角(内翻/外翻/屈伸)截骨术和旋转截骨术。在旋转经转子截骨术中,股骨头颈骨折块的坏死区绕股骨颈轴向前或向后旋转,以移出坏死区。
通过内翻截骨术,坏死病变向内侧移动,而股骨头的外侧(通常是非坏死部分)移动至负重区域。根据矢状位磁共振成像(MRI)序列上坏死的定位,可以执行额外的屈曲或伸展矫正。对于所有手术,准确了解股骨近端的血管解剖对于避免医源性坏死至关重要[11,15]。
优点(股骨近端截骨术治疗股骨头坏死)
• 髋关节外科脱位[4]可以完全接触到髋臼和股骨头。
• 坏死区域的直接治疗可以通过刮除(坏死骨)术、骨移植和软骨损伤治疗来进行。
• 可以进行偏心距矫正、盂唇治疗或股骨扭转角矫正等同期手术[21]。
• 内翻或屈曲截骨术可减少坏死病变处的负荷力并帮助骨骼愈合。
缺点(股骨近端截骨术治疗股骨头坏死)
• 至少8周的限制性负重。
• 手术技术要求高。
• 由于内翻截骨术导致的杠杆臂、肌肉张力和腿长度缩短导致的髋部解剖学变化可能导致跛行。
• 转子螺钉或骨板可能需要二次手术拆除。
适应症(股骨近端截骨术治疗股骨头坏死)
• 股骨头局限性骨坏死。
• 无晚期退行性征象(常规X线片中Tönnis等级 ≤ 1)
• 相对年轻的患者(年龄 < 50 岁)
禁忌症(股骨近端截骨术治疗股骨头坏死)
• X线显示髋关节明显退化(> Tönnis 1级)。
• 广泛性股骨头骨坏死(Kerboul ≥ 240°)
• 晚期病变(骨循环研究协会[ARCO]分期≥ 3b 期)。
• 老年患者(年龄≥ 50 岁)。
患者信息
一般手术风险(血栓形成;肺栓塞;过敏反应;术中定位导致的皮肤、肌肉和神经损伤;皮肤神经损伤伴麻木/感觉迟钝;出血过多需要血液制品输注;伤口愈合延迟和感染)
特定风险(股骨近端截骨术治疗股骨头坏死)
• 尽管进行了手术,但坏死和骨关节炎仍在恶化
• 截骨术或大转子的延迟愈合和假关节形成
• 双侧腿长度差异
• 异位骨化
术前检查
• 充分了解患者的病史(例如,正在进行的类固醇治疗、化疗、酗酒)对于评估是否可以选择保髋手术至关重要
• 标准化的X线成像,包括骨盆前后位射线照相和轴向视图,用于使用模板进行规划
• 髋关节磁共振关节造影,最好通过关节内注射造影剂和腿部牵引来评估坏死的大小和位置以及髋关节内损伤[16]
• 轴位成像(计算机断层扫描[CT]或MRI)用于评估股骨扭转角,以对扭转进行可能的额外矫正
• 股骨截骨方向和程度的术前模板;内翻截骨术将位于内侧的病灶更靠内侧,将未受影响的外侧部分转移到承重区,股骨屈曲截骨术将位于前方的病灶更靠前,将未受影响的后部转移到承重区;可以结合内翻和屈曲截骨术;通常在任何方向上执行不超过20°的校正
工具
用于股骨近端的锁定加压接骨板(儿童髋接骨板;DePuy Synthes,Zuchwil,Switzerland)或用于成人的角形刀片接骨板(DePuy Synthes)
用于软骨治疗的可选纤维蛋白胶(Tissucol;Baxter,Warsaw,Poland)
可选的自体基质诱导软骨形成(AMIC),具有I/III型胶原基质(Chondro-Gide;Geistlich Pharma,Wolhusen,Switzerland)
麻醉和体位
• 全身麻醉,肌肉组织完全放松
• 严格的侧卧位
• 用前后方支撑稳定患者
• 将未受累的小腿放置在隧道枕垫中以避免受压,并为受累的下肢在水平位置安排一个平面
• 消毒和无菌手术单包括整个下肢直至胸部;大转子应该可以自由触及
• 用于术中定位和监测截骨术、角度校正和钢板螺钉放置的X线透视检查
• 单次静脉注射抗生素预防(头孢呋辛)
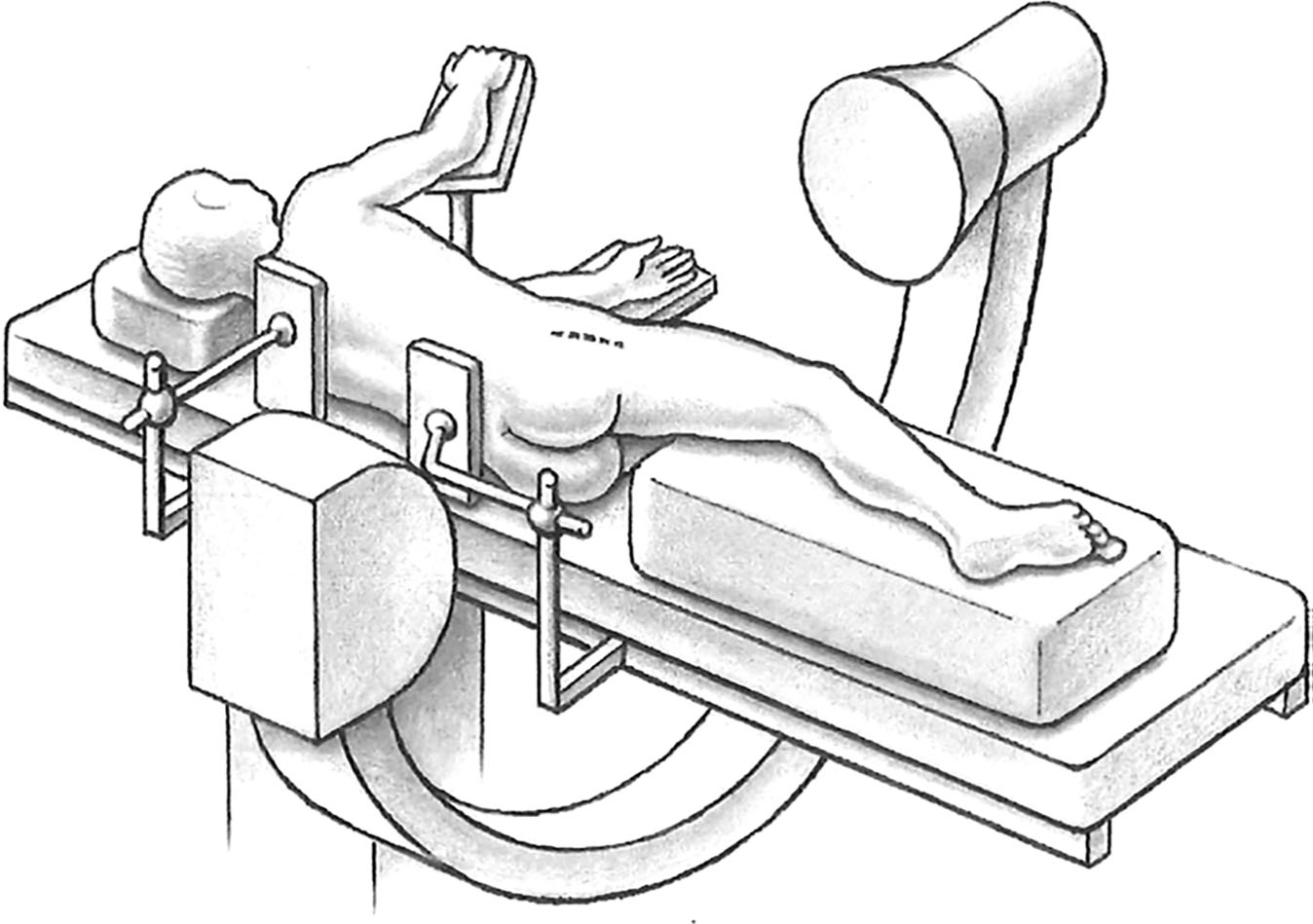
Fig. 1 A straight lateral skin incision of 15–20cmismade, centered over the greater trochanter with the patient in the lateral decubitus position.
图1 一个15-20cm的直的外侧皮肤切口,以大转子为中心,患者处于侧卧位。
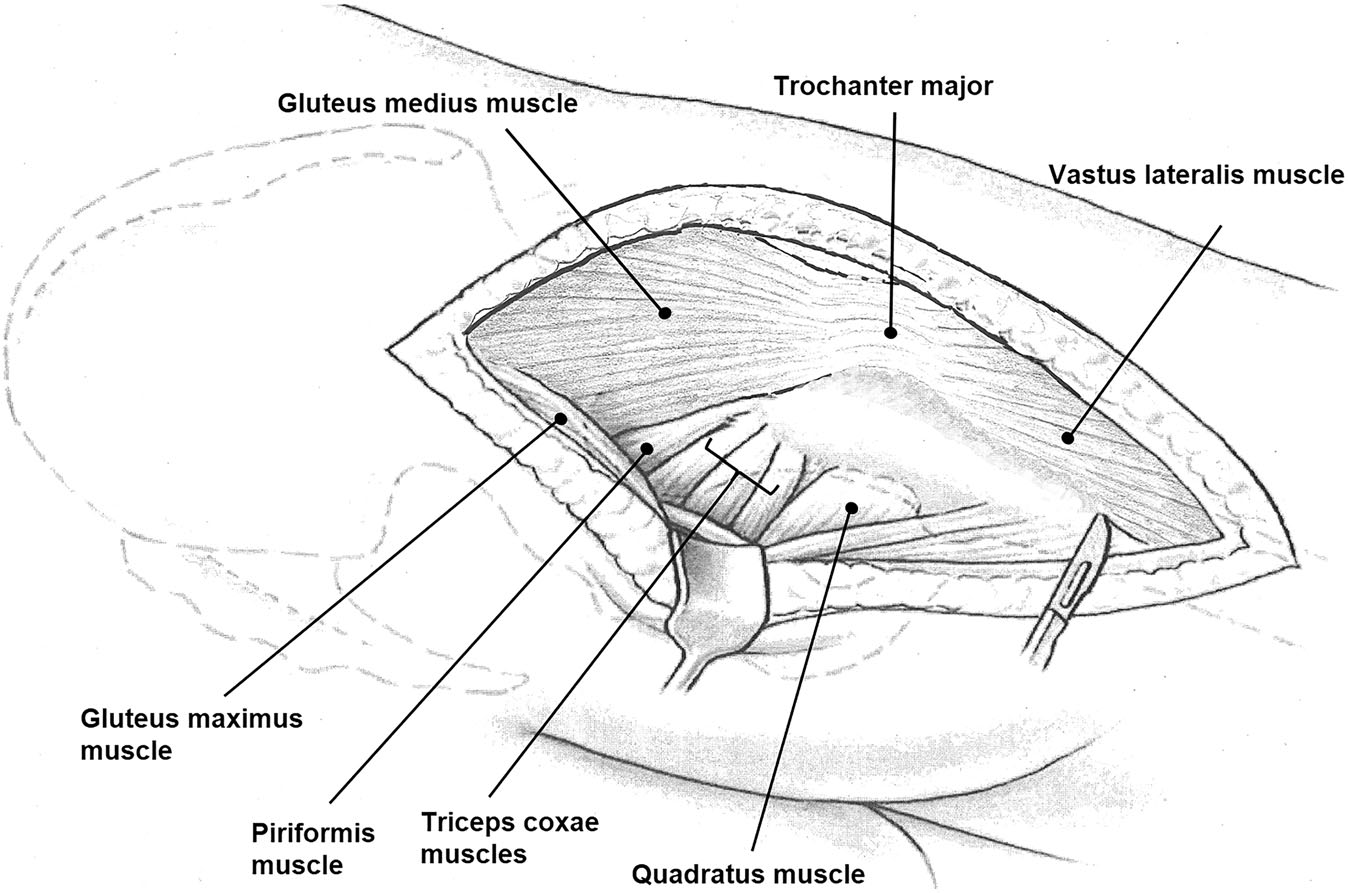
Fig. 2 A surgical hip dislocation is an intermuscular and internerval approach. After incision of the tractus, the superficial interval between the gluteus maximus and gluteus medius (Gibson interval) is developed. The deep interval is between the piriformis and the gluteus minimus muscle and best developed with the hip in extension and internal rotation
图2 髋关节外科脱位是一种肌间和神经间入路。切开髂胫束后,形成臀大肌和臀中肌之间的浅层间隙(Gibson间隙)。深层间隔位于梨状肌和臀小肌之间,在髋关节伸展和内旋时显露最好。
Fig. 3 Typically, a stepped trochanteric osteotomy is performed to minimize the risk of trochanteric pseudarthrosis after refixation. Alternatively, a flat osteotomy can be performed when the greater trochanter has to be distalized, if the varus osteotomy would result in a high riding trochanter [1]. The osteotomy starts at the posterosuperior tip of the greater trochanter and ends 10–15mmdistal to the lateral tubercle. Proximally, the osteotomy should end just anterior to the most posterior insertion of the gluteus medius leaving the short external rotators attached to the proximal femur. The trochanteric fragment is mobilized together with the vastus lateralis, gluteus minimus, and medius muscle ventrally and the capsule is exposed.
图3 通常,进行阶梯式转子截骨术以最大限度地降低再固定后大转子假关节形成的风险。或者,如果内翻截骨术会导致转子向高位滑动,则当必须将大转子远移时,可以进行水平截骨术[1]。截骨术从大转子的后上顶端开始,到外侧结节远端10-15mm处结束。在近端,截骨术应该在臀中肌最后止点之前结束,保留短外旋肌群附着在股骨近端上。转子截骨块与股外侧肌、臀小肌和臀中肌一起向腹侧牵拉,并暴露髋关节囊。
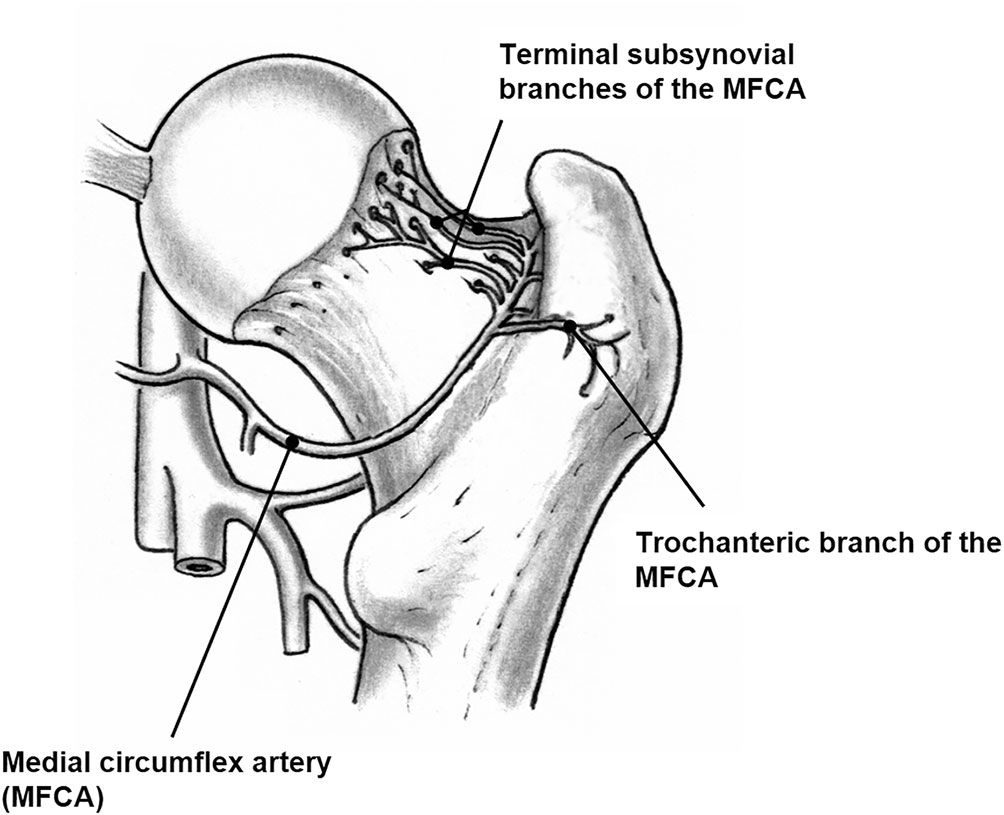
Fig. 4 The vascular anatomy of the proximal femur has to be respected when performing an osteotomy. The main nutrient vessel of the femoral head is the medial branch of the medial femoral circumflex artery (MCFA)
图4 进行截骨术时必须注意股骨近端的血管解剖结构。股骨头的主要营养血管是旋股内侧动脉(MCFA)的内侧支。
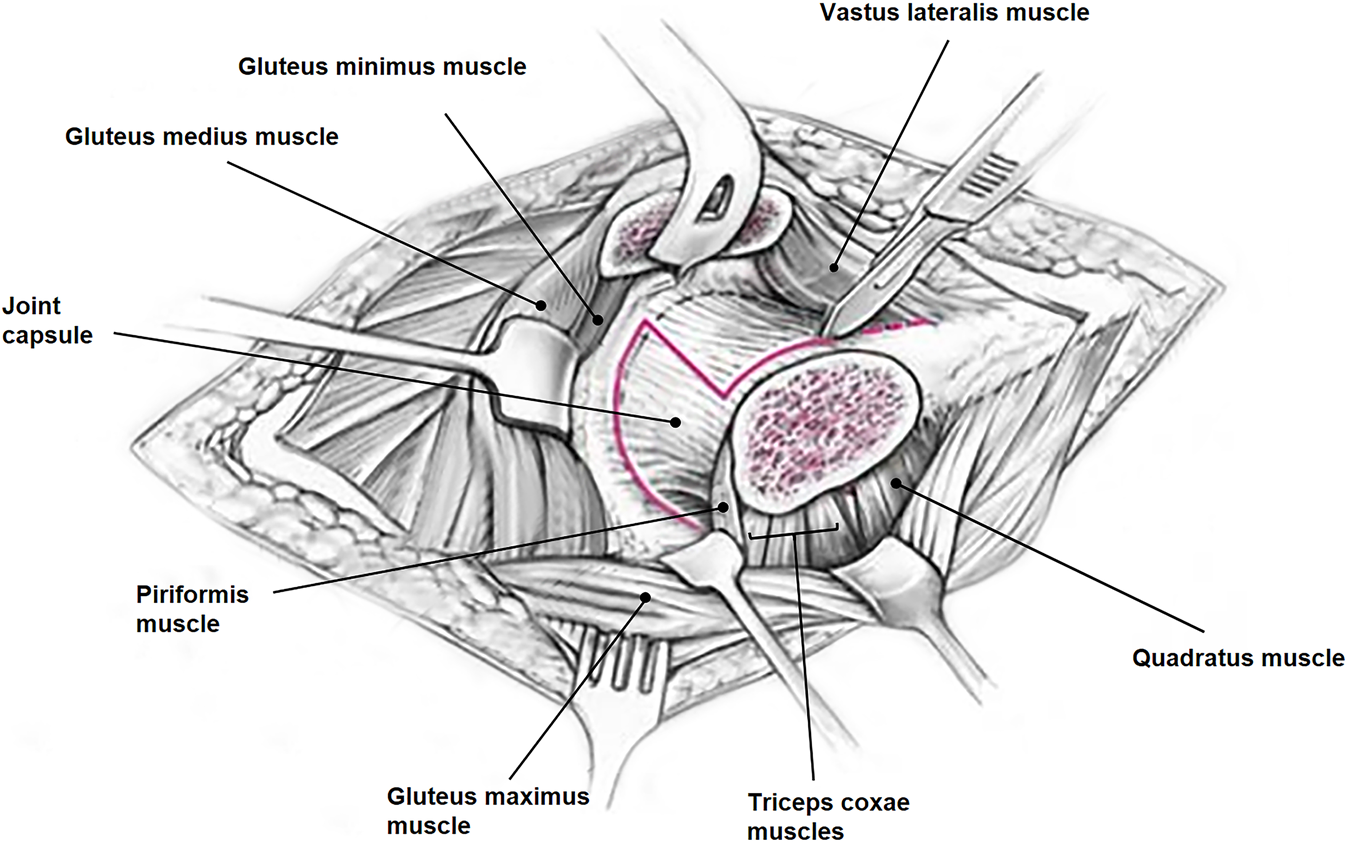
Fig. 5 The capsule is incised in a z-shaped manner without violating the labrum. The ligamentum teres is cut in a subluxed position to allow for full dislocation of the femoral head
图5 在不侵犯髋关节盂唇的情况下,以z字形方式切开髋关节囊。股骨头凹韧带在髋关节半脱位时切断以允许股骨头完全脱位。
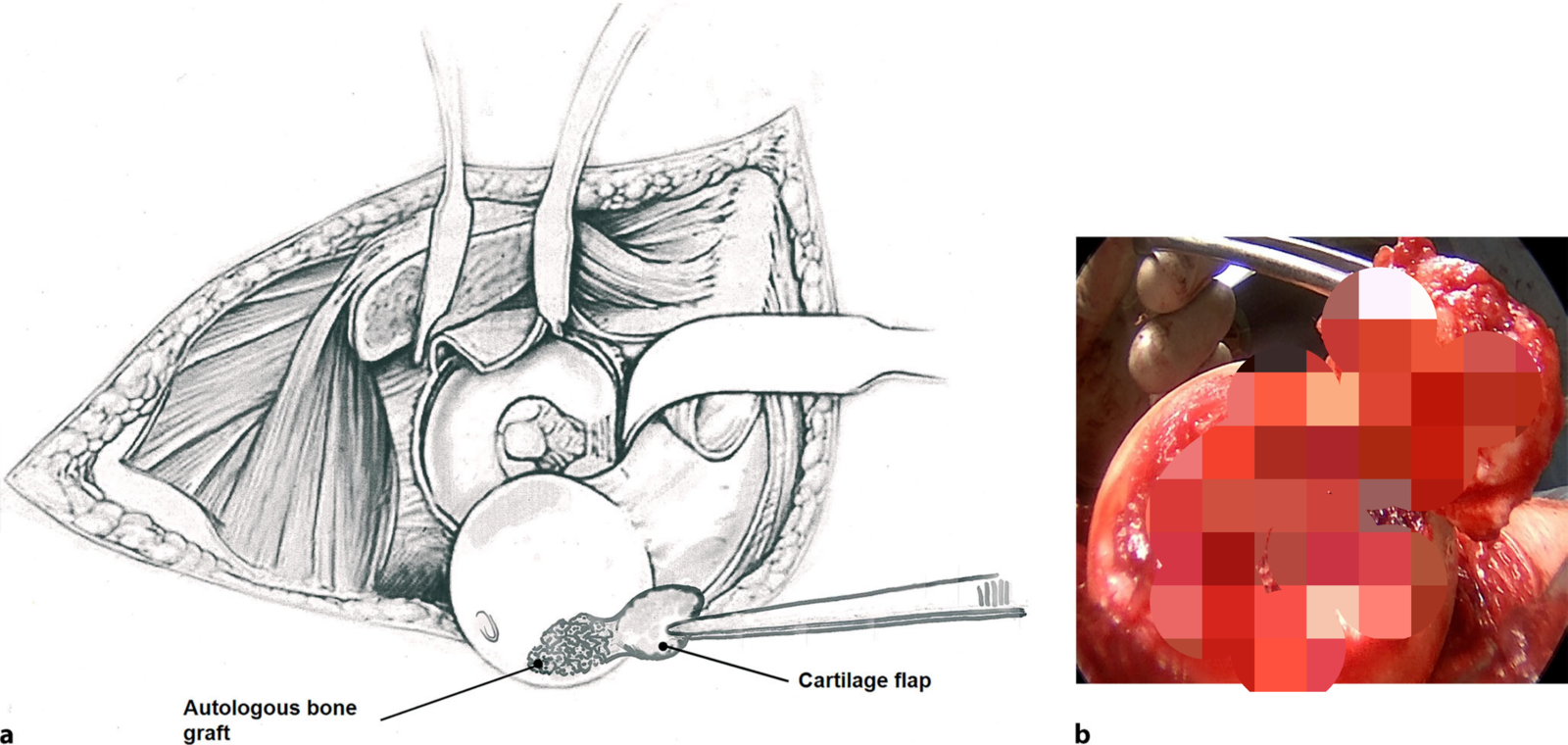
Fig. 6 a The acetabulum and femoral head are inspected. Typically, the cartilage covering the area of the femoral head necrosis is frayed, softened, or detached from the subchondral bone. The cartilage is elevated from the subchondral bone to access the necrotic bone. If not delaminated, an incision of the cartilage at the border of the necrotic area is made. With a high-speed burr, curettage of the necrotic bone is performed. Bone is removed until bleeding cancellous bone is found. Through the trochanteric osteotomy, harvesting of autologous cancellous bone of the trochanter major is performed. b The lesions are filled with impaction bone grafting[19]. Wherever possible, cartilage is preserved by gluing back the previously detached cartilage using fibrin glue and suturing of the cartilage boarder with resorbable monofilament sutures. With a concomitant femoral cartilage defect present, an autologous matrix-induced chondrogenesis (AMIC) is performed. AMIC is used for full cartilage defects, which are then covered with a type I/III collagen matrix (Novocart), glued to the bone with fibrin glue, and attached to the stable cartilage with sutures
图6 a检查了髋臼和股骨头。通常,覆盖股骨头坏死区域的软骨磨损、软化或与软骨下骨分离。软骨从软骨下骨升高以接近坏死骨。如果没有分层,则在坏死区域的边界处切开软骨。使用高速磨刀刮除坏死骨,直到发现出血的松质骨。通过转子截骨术,采集大转子的自体松质骨。b病变充满嵌塞移植骨[19]。在可能的情况下,通过使用纤维蛋白胶粘回先前分离的软骨并用可吸收的单股缝合线缝合以保留软骨。由于存在伴随的股骨软骨缺损,因此进行了自体基质诱导软骨形成(AMIC)。AMIC用于全软骨缺损,然后用I/III型胶原基质(Novocart)覆盖,用纤维蛋白胶粘在骨质上,并用缝线固定在稳定的软骨上。
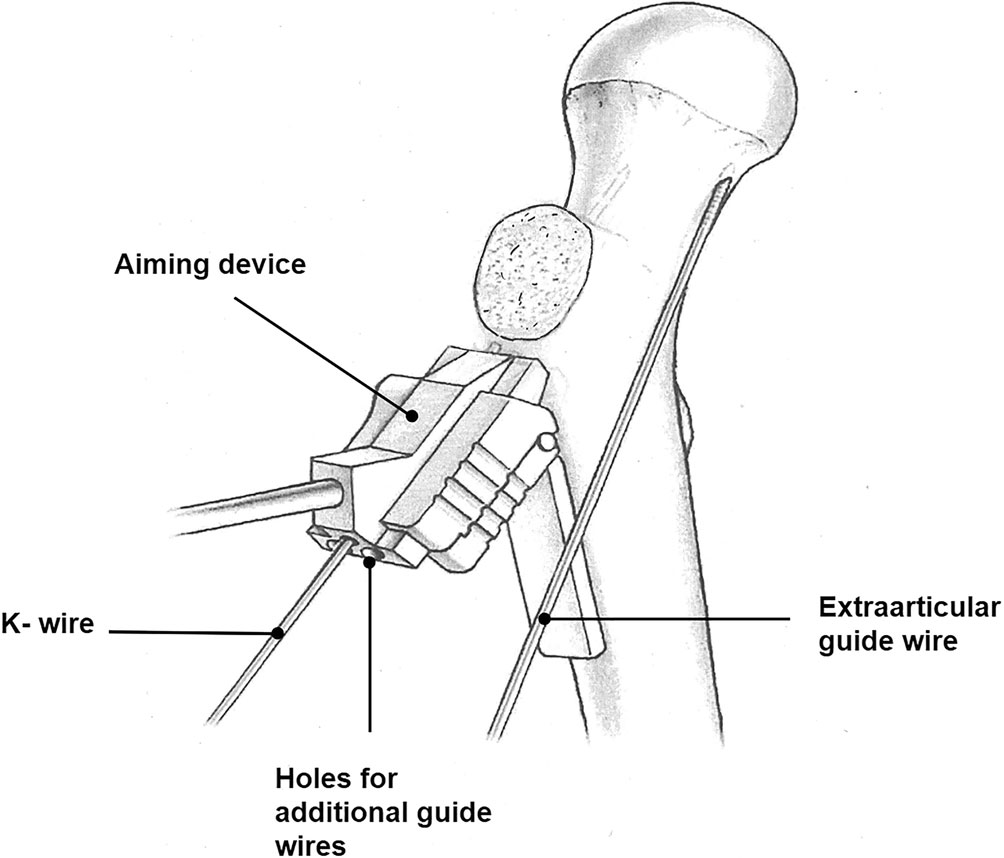
Fig. 7 The first guide wire is placed extra-articularly in line with the axis of the femoral neck. It indicates the femoral antetorsion and the height of the entry point of the positioning Kirschner wire in the sagittal plane. The calculated correction angle has to be adjusted on the aiming block. The aiming block consists of a guide proximally and a wing distally; the wing must be placed parallel to the shaft of the femur. If additional flexion or extension correction is needed, the wing of the aiming block can be placed posterior or anterior on the diaphysis. The positioning Kirschner wire is then inserted through the aiming block and placed in the center of the femoral neck.
图7 第一根导针在关节外与股骨颈的轴线对齐。它表示股骨前倾角和矢状面上定位克氏针进入点的高度。必须在瞄准块上调整计算出的校正角度。瞄准块由近端的导向器和远端的翼部组成;翼部必须平行于股骨干放置。如果需要额外的屈曲或伸展矫正,瞄准块的翼部可以放置在骨干的后部或前部。然后将定位克氏针穿过瞄准块插入并放置在股骨颈的中心。
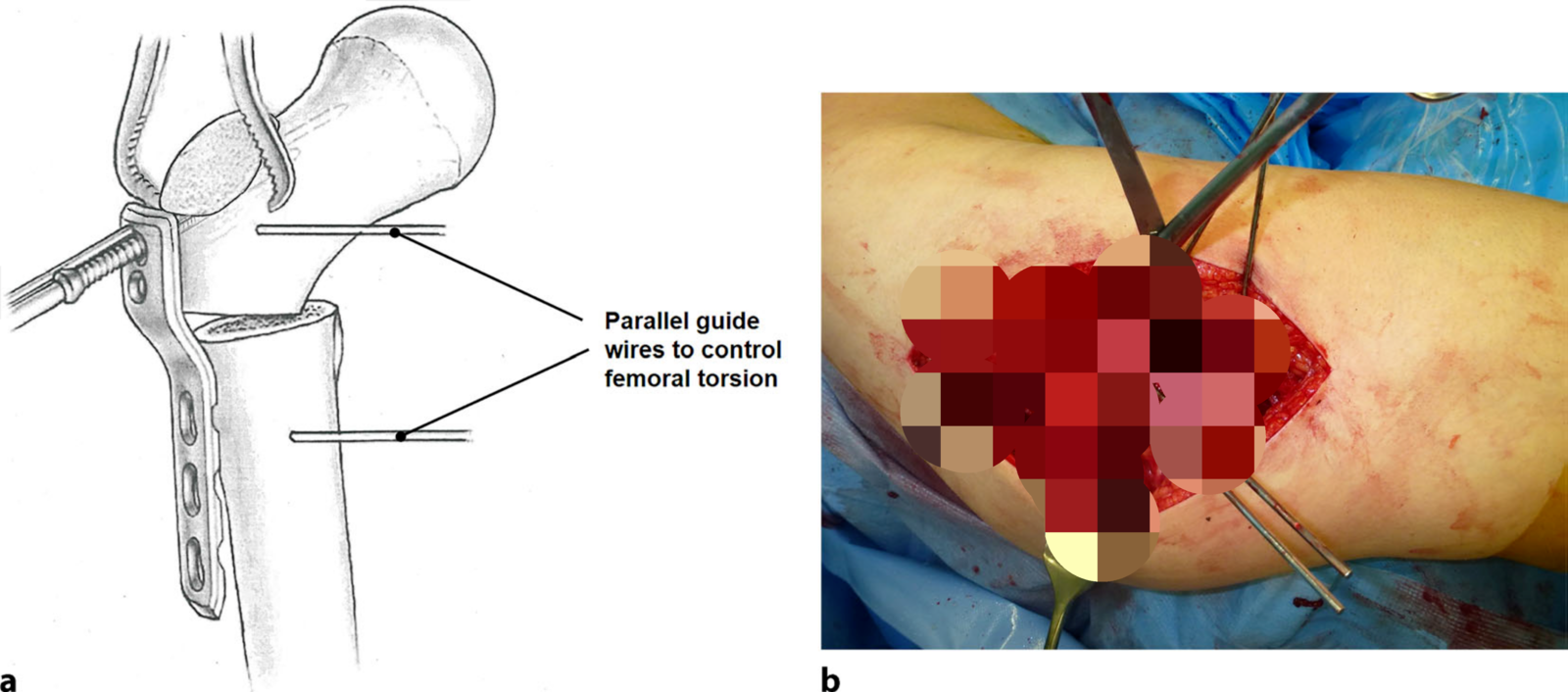
Fig. 8 Two more guide wires are inserted through the holes provided in the aiming block; they will serve as guidewires for the cannulated femoral neck screws. To control the rotation, the anterior cortex is marked with two parallel wires. The osteotomy is typically performed at the intertrochanteric level perpendicular to the shaft under constant irrigation. A varization of 15–20° is usually sufficient. The plate is attached to the proximal fragment with three angular stable and cannulated screws; typically, two of them are placed in the femoral neck, one in the calcar region.
图8 通过瞄准块上的孔插入另外两根导针;它们将用作空心股骨颈螺钉的导针。为了控制旋转,前皮质标有两条平行线。截骨术通常在不断冲洗的情况下在垂直于轴的转子间水平进行。15–20°的变化通常就足够了。用三个角度稳定的空心螺钉将骨板固定在近端骨折块上;通常,其中两个放置在股骨颈,一个在股骨距区域。
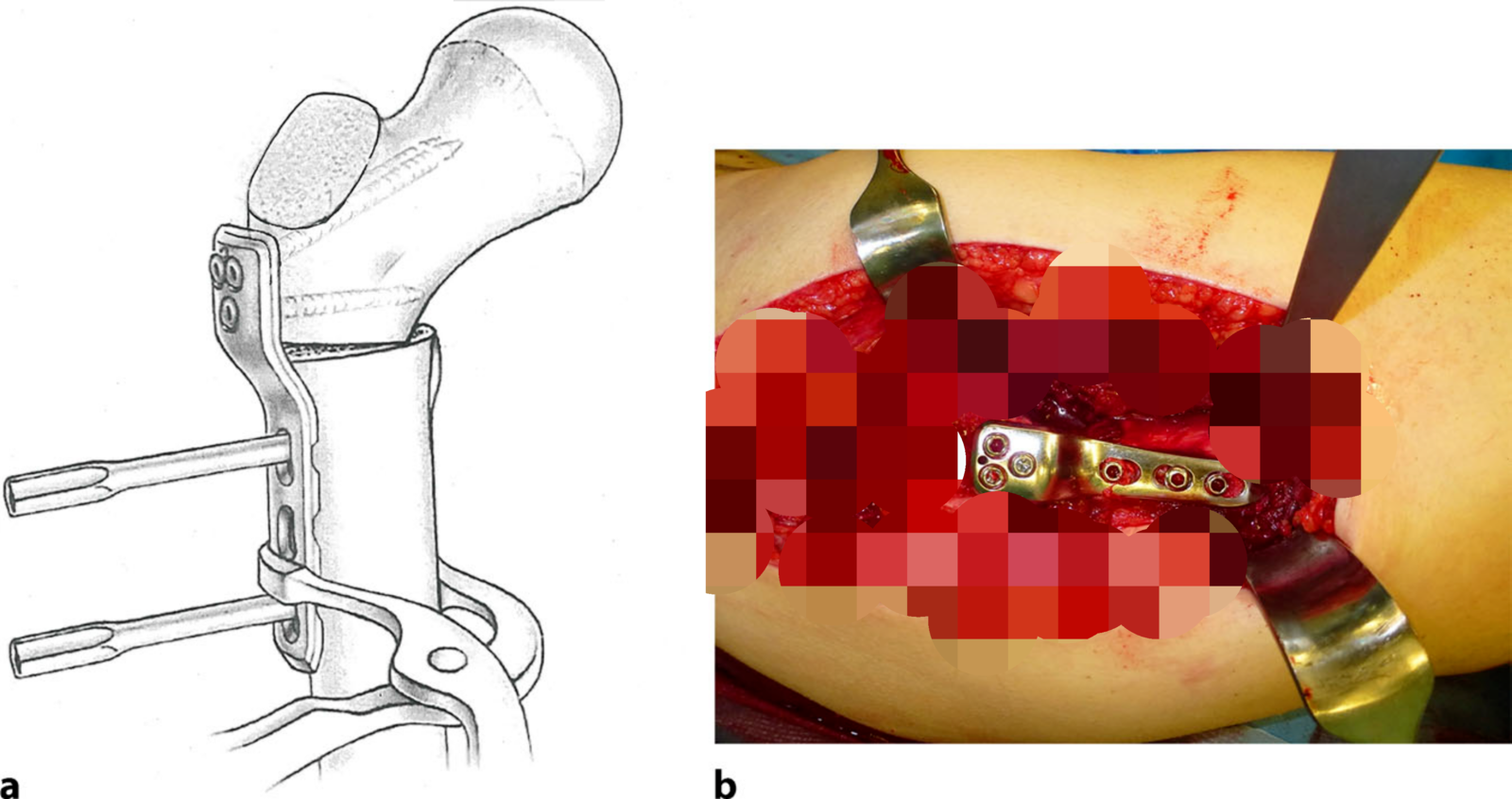
Fig. 9 An implant with offset can be used to prevent additional lateralization of the diaphyseal fragment. The plate is then fixed to the diaphyseal fragment with either locking head or cortical screws.
图9 带偏心距的内固定物可用于防止骨干碎片的额外外侧移位。然后用锁定头或皮质螺钉将钢板固定到骨干骨折块上。
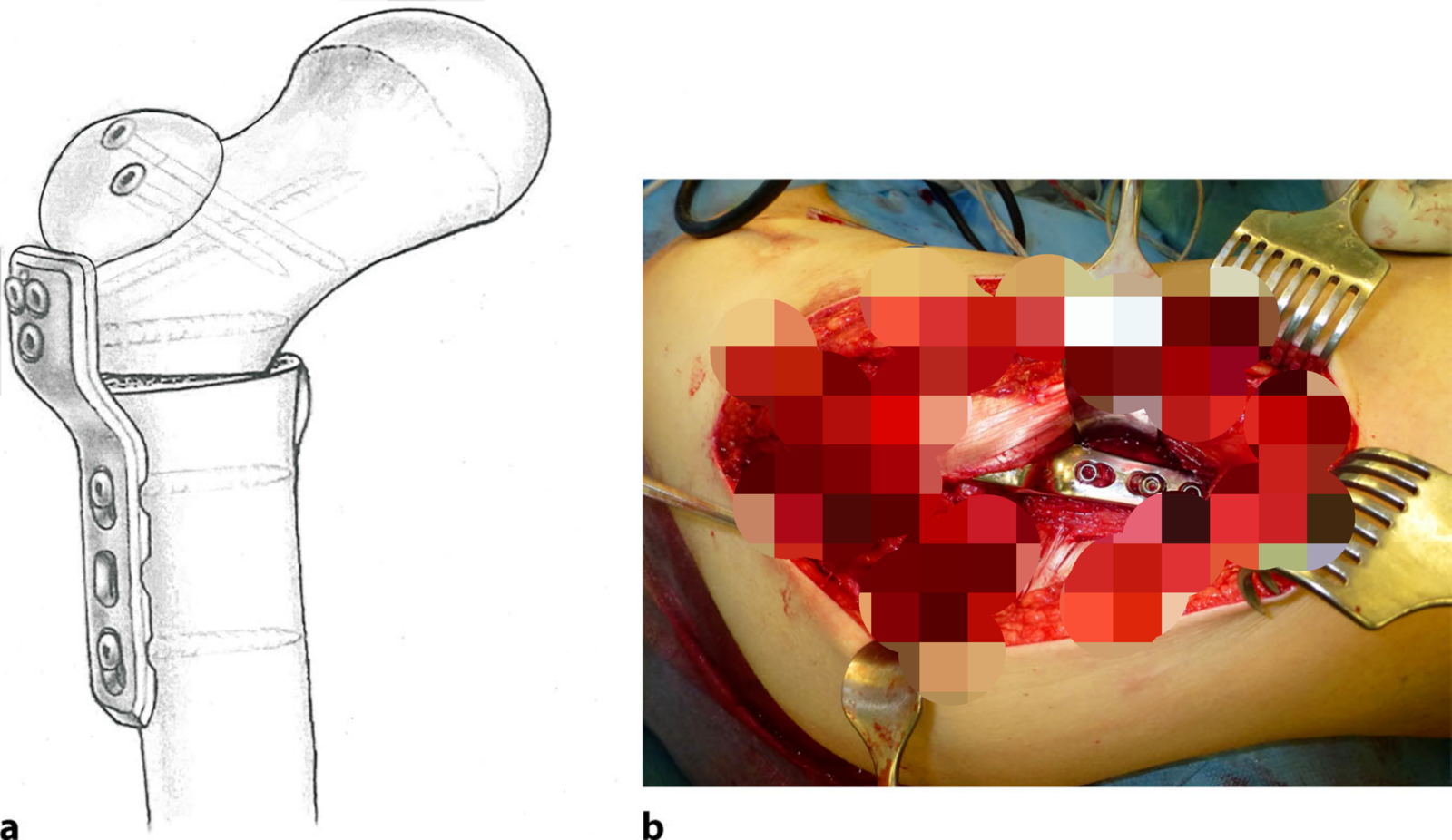
Fig. 10 Fixation of the trochanteric fragment is performed with 3.5-mm cortical screws, optionally in a distalized position to avoid a high riding trochanter.
图10 使用3.5毫米皮质螺钉固定转子骨碎片,可选择在远端位置以避免大转子高位。
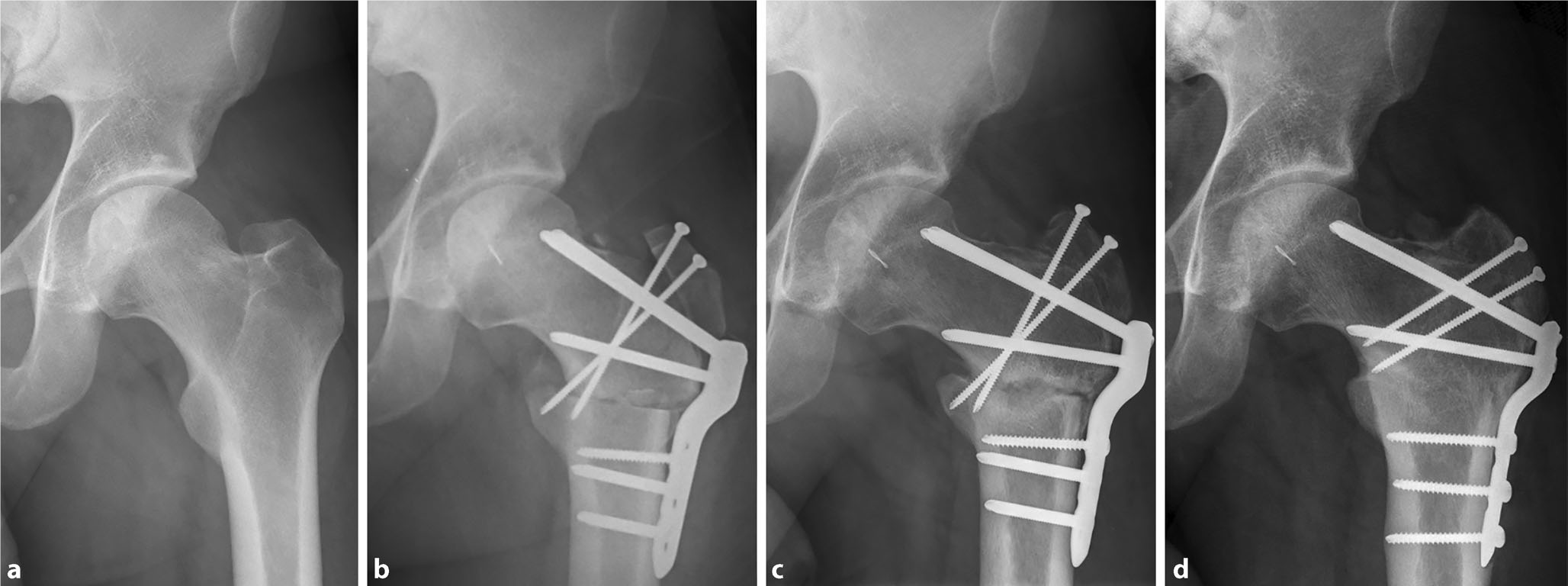
Fig. 11 Exemplary case with re-osteosynthesis of a pseudarthrosis. a Preoperative image with osteonecrosis; b shortly after surgery following varization and trapdoor procedure; c 8months postoperatively with pseudarthrosis of the femoral osteotomy; d 4-year postoperative image after re-osteosynthesis of the osteotomy, maintaining sphericity of the femoral head.
图11 假关节再骨合成的示例性病例。a骨坏死的术前图像;b内翻截骨和活板门手术后不久;c术后8个月,股骨截骨假关节形成;d截骨术再骨化后4年的术后图像,保持股骨头的球形度。
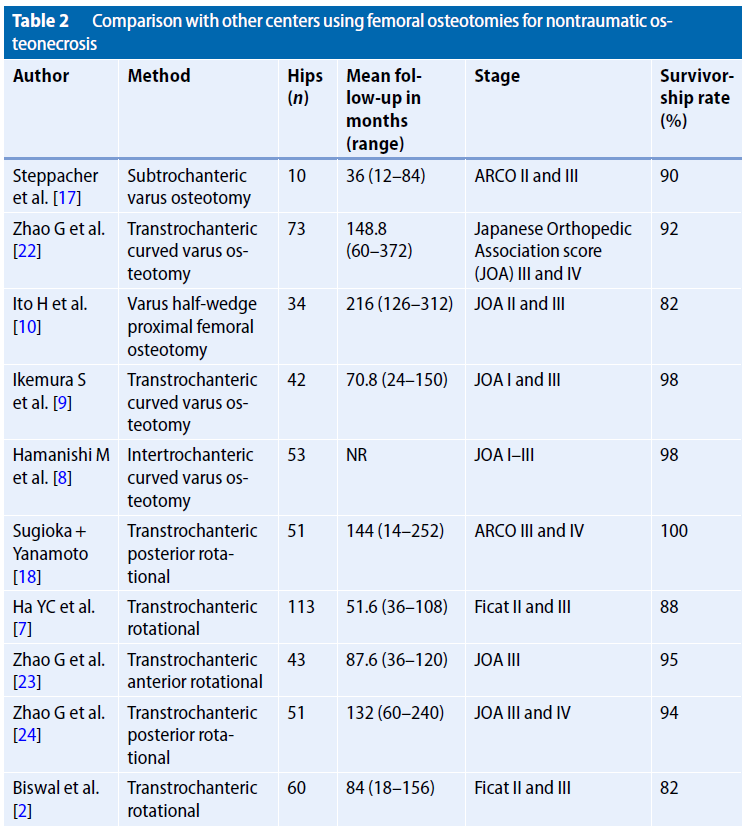
Table 2 Comparison with other centers using femoral osteotomies for nontraumatic osteonecrosis
表2 与使用股骨截骨术治疗非创伤性骨坏死的其他中心的比较
Femoral osteotomies for the treatment of avascular necrosis of the femoral head
Objective: Unloading of the area of necrosis out of the weight-bearing region by shifting healthy bone in the main weight-bearing area, which may delay the progression of the necrosis and enable healing.
Indications: Circumscribed osteonecrosis of the femoral head without advanced degenerative signs (Tönnis grade ≤ 1) in the relatively young patient (age < 50 years).
Contraindications: Radiographic joint degeneration (> Tönnis grade 1); extensive avascular necrosis (Kerboul angle > 240°); advanced lesions (≥ Association Research Circulation Osseous [ARCO] classification 3b).
Surgical technique: By performing a surgical hip dislocation, full access to the hip joint is gained. A femoral varus osteotomy is used to turn the necrotic lesion of the femoral head out of the central weight-bearing area and more medially. Osteosynthesis is performed with an angular stable screw or a blade plate. Via a trapdoor procedure, direct debridement and autologous bone grafting from the trochanter major is possible. The cartilage flap is preserved whenever possible or supplanted by an autologous matrix-induced chondrogenesis (AMIC).
Postoperative management: A passive motion device is installed during hospital stay beginning immediately after surgery to prevent capsular adhesions. After surgery, patients are mobilized with partial weight-bearing of 15 kg with the use of crutches for at least 8 weeks. Forced abduction and adduction as well as flexion of more than 90° are restricted to protect the trochanteric osteotomy. After radiographic confirmation of healing at the 8‑week follow-up, stepwise return to full weight-bearing is allowed and abductor training is initiated.
Results: Nine patients (10 hips) with osteonecrosis of the femoral head were treated with surgical hip dislocation and varus osteotomy. Six hips were treated with autologous bone grafting, four hips with antegrade drilling. Chondral lesions were sutured in four cases, whereas two cases needed an AMIC treatment. The mean age at operation was 29 ± 9 years (20-49), and the mean follow-up time for all patients was 3 ± 2 years (1-7). Conversion to a total hip prosthesis was required for one hip with progressing arthrosis. The other nine hips showed no progression of necrosis and an improved clinical outcome. Complications were pseudarthrosis of the femoral osteotomy and pseudarthrosis of the greater trochanter.
Keywords: Hip dislocation; Osteonecrosis; Osteotomy; Trapdoor procedure; Weight-bearing.
Surgical principle and objective
The aim of femoral osteotomies in the treatment of ONFH is to move the area of necrosis out of the weight-bearing region, which leads to delayed progression or even healing of the necrosis. Femoral osteotomies in the treatment of ONFH can be divided into angular and rotational osteotomies. With a rotational transtrochanteric osteotomy, the necrotic zone of the head-neck fragment is rotated anterior or posterior around the neck axis to unload the necrotic zone.
With a varus angular osteotomy, the necrotic lesion is shifted medially and the lateral, typically non-necrotic part of the femoral head is displaced in the area of weight-loading. Additional flexion or extension correction can be performed, depending on the localization of necrosis on sagittal magnetic resonance imaging (MRI) sequences. For all procedures, precise knowledge of the vascular anatomy of the proximal femur is essential to avoid iatrogenic necrosis [11, 15].
Advantages
· Surgical hip dislocation [4] provides full access to the acetabulum and the femoral head.
· Direct treatment of the necrotic area can be performed with curettage, bone grafting, and treatment of cartilage lesions.
· Concomitant procedures such as offset correction, labral treatment, or correction of femoral torsion can be performed [21].
· A varus or flexion osteotomy decreases the loading force on the necrotic lesion and helps the bone to heal.
Disadvantages
· Minimum 8 weeks of limited weightbearing.
· Technically demanding surgical technique.
· Change in hip anatomy with changes in lever arm, muscular tension, and leg length shortening due to varus osteotomy may lead to limping.
· Trochanteric screws or plate may require secondary hardware removal.
Indications
· Circumscribed osteonecrosis of the femoral head.
· No advanced degenerative signs (Tönnis grade ≤ 1 in the conventional radiograph)
· Relatively young patient (age < 50 years)
Contraindications
· Advanced radiographic joint degeneration (> Tönnis grade 1).
· Extensive osteonecrosis (Kerboul ≥ 240°) Advanced lesions (≥ grade 3b Association Research Circulation Osseous [ARCO] classification).
· Older patients (age ≥ 50 years).
Patient information
General surgical risks (thrombosis; lung embolism; allergic reactions; injuries of skin, muscle, and nerves due to intraoperative positioning; injury of cutaneous nerves with numbness/dysesthesia; excessive bleeding requiring blood products; delayed wound healing and infection)
Specific risks of this procedure:
· Progression of necrosis and osteoarthritis in spite of operation
· Delayed union and pseudarthrosis of the osteotomy or greater trochanter
· Leg length discrepancy
· Heterotopic ossification
Preoperative work-up
· Good knowledge of the patient’s history (e.g., ongoing steroid therapy, chemotherapy, alcohol abuse) is essential to evaluate whether a hip preserving operation is an option.
· Standardized radiographic imaging including anteroposterior pelvic radiograph and axial view for planning with templates.
· Magnetic resonance arthrography of the hip, preferably with intraarticular contrast agent injection and leg traction for evaluation of size and location of the necrosis and the intraarticular damage [16].
· Axial imaging (computed tomography [CT] or MRI) for evaluation of femoral torsion, for possible additional correction of torsion.
· Preoperative templating for the direction and degree of femur osteotomy; varus osteotomy shifts a medially located lesion more medial and the non-affected lateral part into the weight-bearing zone, femoral flexion osteotomy shifts an anteriorly located lesion more anterior and the non-affected posterior part into the weightbearing zone; both varus and flexion osteotomies can be combined; no more than 20° of correction in any direction is usually performed.
Instruments
Locking compression plate for proximal femur (pediatric hip plate; DePuy Synthes, Zuchwil, Switzerland) or angled blade plate for adults (DePuy Synthes).
Optional fibrin glue (Tissucol; Baxter, Warsaw, Poland) for cartilage treatment.
Optional autologous matrix-induced chondrogenesis (AMIC) with type I/III collagen matrix (Chondro-Gide; Geistlich Pharma, Wolhusen, Switzerland).
Anesthesia and positioning
· General anesthesia with full relaxation of the musculature.
· Strict lateral decubitus position.
· Stabilization of patient with two side supports.
· Placement of the uninvolved lower leg in a tunnel bolster to avoid pressure and arrangement of a flat surface in a horizontal position for the involved lower limb.
· Disinfection and sterile drapes include the entire lower extremity up to the thorax; the great trochanter should be freely palpable.
· Fluoroscopy for intraoperative orientation and monitoring of the osteotomy, angular corrections, and placement of hardware.
· Single-shot intravenous antibiotic prophylaxis (cefuroxime).
文献出处:Christiane Sylvia Leibold, Florian Schmaranzer, Klaus-Arno Siebenrock, Simon Damian Steppacher. Femoral osteotomies for the treatment of avascular necrosis of the femoral head. Review, Oper Orthop Traumatol. 2020 Apr;32(2):116-126. doi: 10.1007/s00064-019-00642-x. Epub 2019 Nov 29.
本文是陶可版权所有,未经授权请勿转载。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论