 三甲
三甲
股骨头坏死:病因、诊断及治疗方式:2019英国医学杂志(BMJ)(医学生及低年资住院医师培训之)综述
股骨头坏死:病因、诊断及治疗方式:2019英国医学杂志(BMJ)(医学生及低年资住院医师培训之)综述
作者:Jonathan N Lamb, Colin Holton, Philip O‘Connor, Peter V Giannoudis
作者单位: Leeds Institute of Rheumatic and Musculoskeletal Medicine, School of Medicine, University of Leeds, Leeds, UK.
译者:陶可(北京大学人民医院骨关节科)
股骨头坏死你需要了解什么?
• 股骨头坏死(AVNFH)的常见危险因素包括:酗酒、使用类固醇激素、化疗和免疫抑制剂药物以及镰状细胞性贫血。
• 如果患者髋部疼痛持续超过6周且X线片正常,请考虑对髋部进行核磁共振MRI扫描,并转诊至骨科(保髋治疗)团队。
• 早期治疗可使髋关节7年后存活率提高至88%。

Fig 1 Demonstration of hip rotation to elicit hip pain with the patient sitting (A) and supine (B, C, D).
图1 演示通过患者坐位(A)和仰卧位(B、C、D)引起髋部疼痛的髋关节旋转活动(髋关节查体之内外旋转活动)。
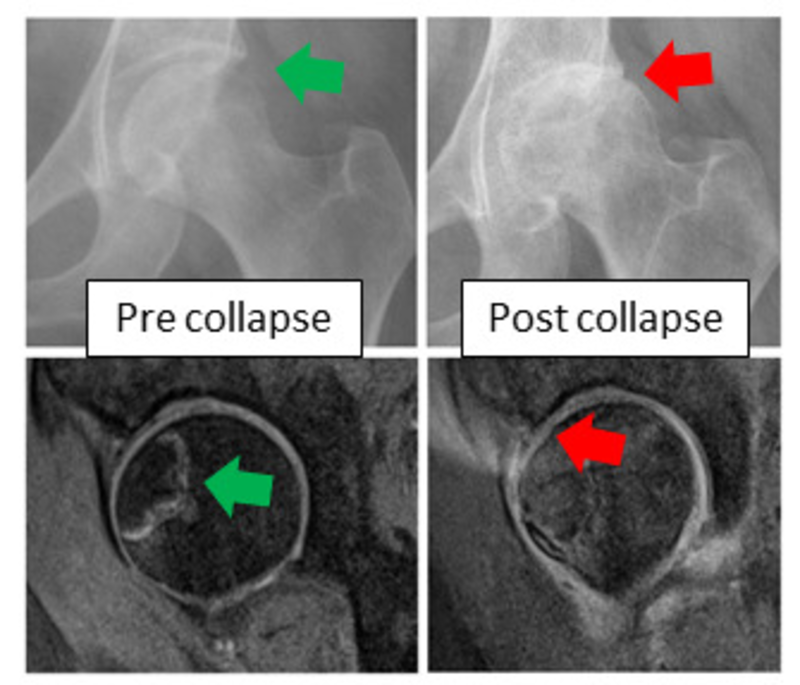
Fig 2 Typical changes seen on plain radiograph (top) and MRI (bottom) of the hip in early and late AVNFH. The appearance of early AVNFH is not apparent on plain radiograph but is visible on MRI.
图2 早期和晚期股骨头坏死(AVNFH)髋关节平片(上)和MRI(下)中看到的典型变化。早期股骨头坏死(AVNFH)的在平片上表现不明显,但在MRI上可见明显信号的改变。
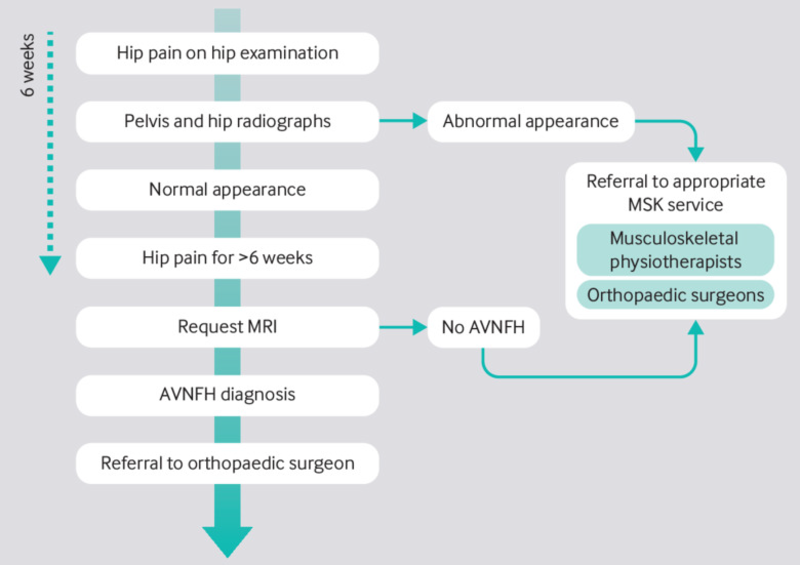
Fig 3 Proposed pathway for managing AVNFH in a primary care setting.
图3 在基层医疗机构中管理股骨头坏死(AVNFH)的建议诊治流程。
典型病例:
一名36岁的女性向她的全科医生报告,有左侧腹股沟疼痛放射到膝盖的病史。疼痛很严重,走路时更严重,并伴有跛行。一年后,患者再次去看全科医生,尽管进行了镇痛,但疼痛仍持续存在。髋关节和膝关节的平片显示髋关节间隙轻微变窄,没有其他特征,她被转诊到二级骨科诊所。髋关节磁共振成像(MRI)扫描显示股骨头缺血性坏死(AVNFH)伴塌陷的典型特征。
什么是股骨头缺血性坏死?
股骨头坏死(AVNFH)由于微循环异常而导致软骨下骨结构完整性丧失。潜在的发病机制尚不清楚;风险因素可能会以某种方式影响微循环,但这尚未得到研究证实。共同的终点是微循环异常和坏死。软骨下骨随后塌陷,导致进行性、继发性髋关节骨关节炎。
在英国,平均发病年龄为58.3岁,每10万名患者中有2人患病。平均而言,股骨头坏死(AVNFH)比典型骨关节炎发生得更早。它在男性中更为常见,发病率最高的是25至44岁的男性和55至75.3岁的女性。在英国,它是50.4岁以下人群全髋关节置换术的第三大常见适应症。
以下因素与股骨头坏死(AVNFH)风险增加相关:
•血液甘油三酯、总胆固醇、低密度脂蛋白胆固醇和非高密度脂蛋白胆固醇水平高;
•男性;
•城市居民;
•股骨头坏死(AVNFH)家族史;
•大量吸烟;
•滥用酒精;
•超重;
•凝血病;
•血管病变;
•艾滋病病毒;
•大量接触类固醇激素、化疗和免疫抑制药物。
类固醇激素已被证明会使骨坏死(非部位特异性)的几率增加3倍,而免疫抑制剂则增加6倍。Zhao报告称,服用皮质类固醇激素的患者发生股骨头坏死(AVNFH)的几率高出35倍,患有“酗酒”状态的患者则高出6倍。
为什么股骨头坏死(AVNFH)会漏诊呢?
股骨头坏死(AVNFH)很少见。患有这种疾病的患者可能同时患有慢性风湿病和血液病。这可能会导致诊断的不确定性,特别是考虑到在这些情况下使用化疗、免疫调节剂和类固醇激素时,这些都是股骨头坏死(AVNFH)的危险因素。
查体可以帮助识别可能引起疼痛的解剖结构,因为髋关节疼痛可能源自髋关节和非髋关节的多个部位。临床表现可能会被错过,因为由于时间和空间的限制,在基层医疗机构中准确确定单纯由于髋关节运动时造成的腹股沟疼痛可能具有挑战性(比较困难)。
股骨头坏死(AVNFH)早期阶段的正常X线片可能会错误地让人放心并延迟适当的转诊。如果X线片呈阴性并且患者继续抱怨髋关节疼痛,医生可能会诊断为非特异性髋关节疼痛(考虑到肌肉骨骼的原因)并建议患者接受物理治疗。
在新发病例中,18.75%只能通过MRI进行诊断,并且在普通X线片上很容易被漏诊。只有MRI扫描才具有诊断意义。
为什么及早确诊股骨头坏死(AVNFH)很重要?
早期诊断和转诊至关重要,因为骨质破坏通常发生在发病后2年内,因此不可能进行保留髋关节的治疗干预(保髋治疗在股骨头坏死发病2年内)。股骨头坏死(AVNFH)的早期发现使多学科团队有时间改变可能引发股骨头坏死(AVNFH)发作的治疗方法。股骨头髓心减压术可降低中短期内进一步手术的需要,但仅适用于疾病的最早阶段。一旦患者进展为继发性髋关节骨关节炎,关节置换通常是不可避免的。
然而,考虑到股骨头坏死(AVNFH)患者年龄较小,翻修手术和相关发病率的终生风险很大。
如何诊断股骨头坏死(AVNFH)?
股骨头坏死(AVNFH)诊断从仔细询问病史和检查开始,以确定髋关节疼痛的来源。最终需要MRI来诊断股骨头坏死(AVNFH),并且还可以诊断髋关节疼痛的其他原因。
仔细的询问病史
病史显示疼痛持续超过6周,通常位于腹股沟和大腿,负重和运动时疼痛更严重。通常没有外伤史。询问危险因素,如果患者有任何“危险信号”,请进行髋关节MRI检查。股骨头坏死(AVNFH)通常是双侧的,双侧股骨头坏死(AVNFH)的风险通常是在单侧确诊后的2年内。
框 1:需要转介或进一步评估的危险信号:
• 髋关节X线检查正常,髋关节疼痛超过6周;
• 患有髋关节疼痛和危险因素的患者,包括:
o 既往单侧股骨头坏死(AVNFH),
o 酗酒,
o 大量接受类固醇激素治疗,
o 免疫治疗,
Ø 化疗,
o 镰状细胞病和其他凝血病,
Ø 艾滋病毒,
o 新近妊娠。
查体
腹股沟、大腿和膝关节前侧疼痛的再现并伴有单独的大腿旋转不能诊断股骨头坏死(AVNFH),但有助于区分髋关节疼痛与脊柱和膝关节疼痛。这可以在患者坐位或仰卧时进行(图1)。
影像学检查
早期股骨头坏死(AVNFH)在X线片上并不明显。如果患者持续感到疼痛,则需要进一步检查和转诊。股骨头坏死(AVNFH)通过髋关节MRI进行诊断,当与临床症状密切相关时,还可以诊断各种可治疗的髋关节疼痛(例如风湿病、肌腱疾病和骨病)(图2)。
仅当有其他原因或高度怀疑风湿病或感染时,才应考虑进行其他检查,例如血液检查。
转诊
如果患者的髋关节MRI显示有股骨头坏死(AVNFH)改变时,请就诊于骨科医生(图3)。
在二级医疗机构就诊时,股骨头坏死(AVNFH)诊断应与开具类固醇激素、化疗和免疫治疗原发病的任何治疗团队共享。
药物和手术治疗取决于患者的特征和股骨头坏死(AVNFH)的阶段。使用前列环素类似物和双膦酸盐对塌陷前股骨头坏死(AVNFH),可以减轻症状并防止关节形合度破坏,但其疗效目前尚不清楚。
手术治疗仍存在争议,但大多数塌陷前股骨头坏死(AVNFH)患者均接受髓心减压手术,并辅以或不辅以药物治疗,以减轻疼痛,并有可能在长达7年的时间里避免88%的患者进行全髋关节置换术治疗。
术后恢复包括12个月的非负重康复锻炼,并在8周后逐渐恢复工作和驾驶。
通常在术后12个月即可感受到完全的治疗益处。专业的三级医疗机构可以提供新的治疗方法,例如骨移植和截骨术,以分别促进血管再生和减轻受损髋关节表面的负荷。一旦发生塌陷,全髋关节置换术可以为患者提供快速、可靠的疼痛缓解和功能改善,但与未来有髋关节翻修的风险,特别是对于年轻患者。
Avascular necrosis of the hip
What you need to know
• Common risk factors for AVNFH are alcoholism, use of steroids, chemotherapy and immunosuppressant medication, and sickle cell anaemia.
• Consider MRI scan of the hip and referral to an orthopaedic team if a patient has a painful hip for longer than six weeks with normal radiographs.
• Early treatment improves the chances of hip survival by up to 88% at seven years.
A 36 year old woman presents to her GP with a history of left groin pain radiating to the knee. The pain is severe, worse on walking, and associated with a limp. The patient revisits the GP a year later with persistent pain despite analgesia. Plain radiographs of the hip and knee show slight narrowing of the hip joint space with no other features and she is referred to a secondary care orthopaedic clinic. A magnetic resonance imaging (MRI) scan of the hip shows classic features of avascular necrosis of the femoral head (AVNFH) with collapse.
What is avascular necrosis of the femoral head?
Osteonecrosis of the femoral head (AVNFH) causes loss of integrity of subchondral bone structure due to abnormal microcirculation. The underlying pathogenesis is unclear1; risk factors are likely to affect microcirculation in some way but this has not been confirmed by research. The common end point is abnormal microcirculation and necrosis. Subchondral bone subsequently collapses, which leads to progressive secondary arthritis.
Mean age of presentation in the UK is 58.3 years, with a prevalence of two per 100 000 patients.2 On average, AVNFH occurs earlier in life than typical osteoarthritis. It is more common in men and the highest prevalence is in men aged 25 to 44 and women aged 55 to 75.3 In the UK it is the third most common indication for total hip replacement in people under 50.4
The following factors are associated with an increased risk of AVNFH3 5:
•High levels of blood triglycerides, total cholesterol, low density lipoprotein cholesterol, and non-high density lipoprotein cholesterol
•Male sex
•Urban residence
•Family history of AVNFH
•Heavy smoking
•Alcohol abuse
•Overweight
•Coagulopathies
•Vasculopathies
•HIV
•High exposure to steroids, chemotherapy, and immunosuppressant medication.
Steroids have been shown to increase odds of osteonecrosis (non-site specific) by a factor of three and immunosuppressants by a factor of six. Zhao reported that the odds of AVNFH were 35 times greater in patients taking corticosteroids and six times greater in patients with “alcoholism” status.3
Why is it missed?
AVNFH is rare. Patients with the condition can have coexisting chronic rheumatic and haematological problems. This may lead to diagnostic uncertainty, particularly given the use of chemotherapy, immunomodulatory agents, and steroids in these conditions, which are all risk factors for AVNFH.
A physical examination can help identify the anatomical structures that might be causing the pain, since hip pain can originate from multiple hip and non-hip areas. Presentations may be missed because accurate reproduction of groin pain on isolated hip movements can be challenging to elicit in a primary care setting due to time and space constraints.
Normal plain radiographs in the early stages of AVNFH can be falsely reassuring and delay appropriate referral. If the plain radiograph is negative and the patient continues to complain of hip pain, the doctor may give a diagnosis of non-specific hip pain (given that musculoskeletal presentations are common in primary care) and send the patient for physiotherapy.
Of new presentations, 18.75% are diagnosable only with MRI and are easily missed on normal plain radiographs.3 Only the MRI scan is diagnostic.
Why does it matter?
Early diagnosis and referral are essential since bone destruction normally occurs within two years of disease onset, making joint preserving intervention impossible.6 Early identification of AVNFH gives the multidisciplinary team time to change medical treatments which might be provoking onset of AVNFH. Surgical decompression of the femoral head reduces the need for further surgery in the short to medium term but is only suitable for the earliest stages of disease.5 Once patients have progressed to secondary hip arthritis, joint replacement is usually inevitable.
However, given the younger age of patients with AVNFH, the lifetime risk of revision surgery and associated morbidity is great.
How is AVNFH diagnosed?
AVNFH diagnosis starts with a careful history and examination to determine that the hip is the source of pain. Ultimately an MRI is required to diagnose AVNFH and may also diagnose other causes of hip pain.
A careful history
A history showing pain lasting longer than six weeks, typically located in the groin and thigh and which is worse on weight bearing and movement is key.6 Usually there is no history of trauma. Ask about risk factors and refer for MRI of the hip if the patient has any “red flags” (box 1). AVNFH is often bilateral and the risk of bilateral AVNFH is highest within two years of unilateral diagnosis.6
Box 1: Red flags requiring referral or further assessment
• Hip pain for more than six weeks with normal hip radiograph
• Patients presenting with hip pain and risk factors including
o previous unilateral AVNFH
o alcohol excess
o high exposure to steroid therapy
o immunologic therapy
o chemotherapy
o sickle cell disease and other coagulopathies
o HIV
o recent pregnancy
Examination
Reproduction of pain in the groin, thigh, and anterior aspect of knee with isolated thigh rotation will not diagnose AVNFH, but will help to differentiate hip pain from pain originating from the spine and knee. This can be performed with the patient sitting
or supine (fig 1).
Radiological tests
Early AVNFH is not apparent on plain radiographs. If the patient continues to be in pain, further investigation and referral is warranted. AVNFH is diagnosed on MRI of the hips,7 which may also diagnose a breadth of treatable hip pain (such as rheumatological disease, musculotendinous disease, and bony disease) when carefully correlated with clinical symptoms8 (fig 2).
Other investigations, such as blood tests, should only be considered if indicated for other reasons or if there is a high suspicion of rheumatological disease or infection.
Referral
If the patient has signs of AVNFH on MRI of the hip, refer to an orthopaedic surgeon for consultation (fig 3).
In secondary care, AVNFH diagnosis should be shared with any care teams involved in the administration of steroids, chemotherapy, and immunologic therapy.
Medical and surgical treatment depend on the patient characteristics and stage of AVNFH. Medical treatment of pre-collapse disease with prostacyclin analogues and bisphosphonates may reduce symptoms and prevent loss of joint congruity but their efficacy is not currently well defined.6
Surgically, treatment remains controversial, but most patients with pre-collapse AVNFH are offered core decompression surgery with or without adjunctive pharmacological therapy to reduce pain and potentially prevent the need for total hip replacement in 88% of patients for up to seven years.9 10
Postoperative recovery involves a period of non-weight bearing for 12 months and gradual return to work and driving at 8 weeks.
Full benefit is usually felt at 12 months after surgery. Specialist tertiary centres may offer novel treatments such as bone grafting and osteotomies to encourage vascular regrowth and unload damaged hip articular surface, respectively. Once collapse has occurred, total hip replacement can give patients rapid, reliable pain relief and improved function but is associated with the risk of future revision, particularly in younger patients. A full description of all the options is beyond the scope of this article and patients should discuss all available options with their surgeon to enable informed shared decision making.
文献出处:Jonathan N Lamb, Colin Holton, Philip O‘Connor, Peter V Giannoudis. Avascular necrosis of the hip. BMJ. 2019 May 30;365:l2178. doi: 10.1136/bmj.l2178.
本文是陶可版权所有,未经授权请勿转载。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论