 三甲
三甲
股骨头坏死:基础知识2019年(致每一位曾经或正在遭受股骨头坏死折磨的病患,都需要了解的科学知识)
股骨头坏死:基础知识2019年(致每一位曾经或正在遭受股骨头坏死折磨的病患,都需要了解的科学知识)
作者:Michelle J Lespasio, Nipun Sodhi, Michael A Mont.
作者单位: Department of Orthopedic Surgery, Boston Medical Center, MA.
译者:陶可(北京大学人民医院骨关节科)
摘要
在本报告中,我们对骨股骨头坏死进行了简明且最新的回顾,股骨头骨坏死是一种病理性、疼痛性且常常致残的疾病,据报道是由于受影响的骨骼区域的血液供应暂时或永久中断造成的。我们将讨论髋关节股骨头骨坏死的流行病学(疾病分布)、发病机制(发展机制)、病因(相关危险因素、原因和疾病)、临床表现(报告的症状和查体结果)、诊断和分类以及治疗方案。
Connections
Every activity of the living organism is connected with a separate part of the body whence it arises. Therefore, an activity is necessarily damaged when the part which produces it is affected.
— Galen of Pergamon, 130 AD-210 AD, prominent Greek physician, surgeon, and philosopher in the Roman Empire
生物体的每项活动都与其产生该活动的身体的一个单独部分相关。因此,当产生某项活动的部分受到影响时,该活动必然会受到损害。
— 佩加蒙的盖伦,公元130年至公元210年,罗马帝国著名的希腊内科医生、外科医生和哲学家
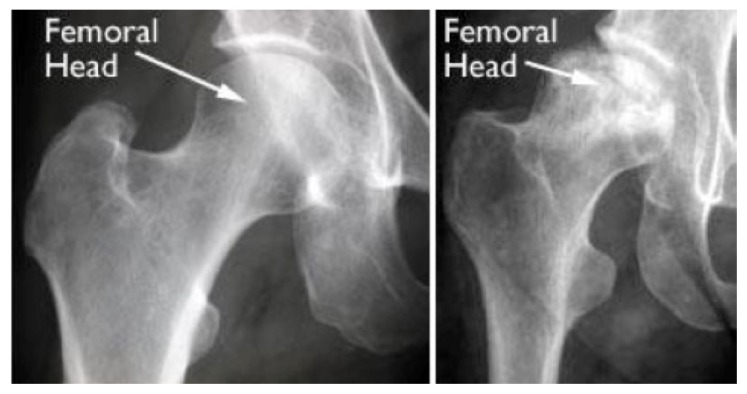
Figure 1 Left, radiograph of a healthy hip joint. Right, radiograph of a hip joint where the osteonecrosis has progressed to collapse of the femoral head.
图1 左图是健康髋关节的X线片;右图是髋关节股骨头坏死已发展到塌陷阶段的X线片。
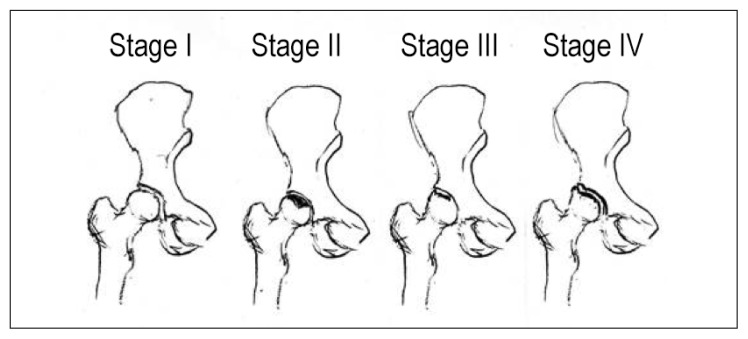
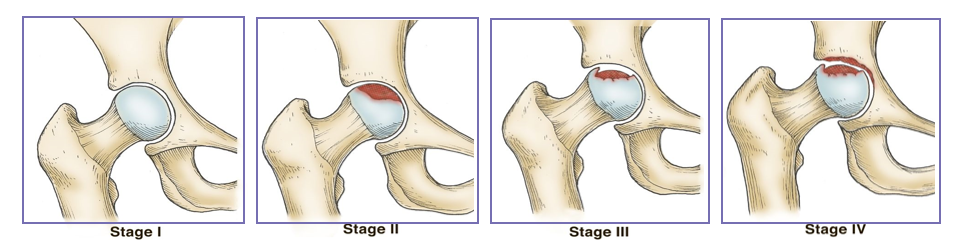
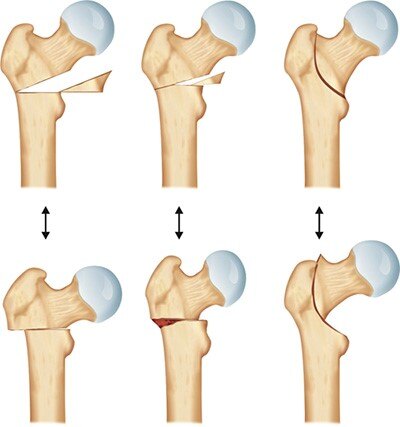
Figure 2 Progression of osteonecrosis using the Ficat & Arlet classification system. Osteonecrosis can progress from a normal, healthy hip (Stage I) to the collapse of the femoral head (Stage IV).
图2 使用Ficat和Arlet分类系统的股骨头骨坏死进展情况。股骨头骨坏死可以从正常、健康的髋关节(第一阶段)发展到股骨头塌陷(并骨关节炎)(第四阶段)。
介绍
本文的目的是介绍影响股骨头或髋关节的骨坏死(ON)的最新情况,以及如何在成年人群中最好地治疗该病。具体来说,本报告将涵盖髋关节股骨头坏死(ON)的流行病学、发病机制、病因、临床表现、诊断和分类以及治疗方案。股骨头坏死(ON),也称为缺血性坏死、无菌性坏死或缺血性骨坏死,与许多导致成熟骨细胞死亡的疾病和危险因素有关,从而导致骨破坏(例如塌陷)或终末期髋关节骨关节炎。这种情况可能发生在身体的任何骨骼(例如上肢、膝关节、肩关节和脚踝关节),或者在不同时间发生在超过1处骨骼,但最常见的是影响髋关节。当最初在髋关节以外的区域进行诊断时,应同时对髋关节进行临床评估以及放射线和其他影像学研究。股骨头坏死(ON)的原因分为外伤性(与损伤相关)或非外伤性(与损伤无关)。准确诊断和分类股骨头坏死(ON)对于帮助指导治疗选择非常重要。识别相关风险因素和患者教育对于成功治疗股骨头坏死(ON)非常重要。针对相关危险因素、药物管理和/或手术,包括关节保留手术和全髋关节置换术(THA),在股骨头坏死(ON)患者的临床管理中也发挥着重要作用。
髋关节股骨头坏死的流行病学
尽管股骨头坏死(ON)的确切患病率尚不清楚,但据估计,美国每年有20,000至30,000名新诊断患者。在美国,约10%的THA患者的诊断是股骨头坏死(ON)。股骨头坏死(ON)影响所有年龄段的人,但最常见于30至65岁之间的患者。诊断时的平均年龄通常小于50岁。男女比例因相关合并症而异。例如,与酒精相关的股骨头坏死(ON)是在男性中更常见,而与系统性红斑狼疮(SLE)相关的股骨头坏死(ON)是在女性中更常见。
每年有超过20,000人因髋关节股骨头坏死需要住院治疗。在许多病例中,双侧髋关节都受到影响。通常,股骨头坏死(ON)会影响股骨头及颈部(近端骨骺)。
髋关节股骨头骨坏死的发病机制/假说
髋关节股骨头坏死(ON)发生的机制仍不清楚。在大多数情况下,股骨头坏死(ON)被认为是遗传倾向、代谢因素和影响血液供应的局部因素(包括血管损伤、骨内压升高和机械应力)综合作用的结果。大多数专家都认为产生干细胞和血小板的股骨头和骨髓缺乏血液供应,导致骨细胞(成熟骨内的细胞)和/或间充质细胞(形成软骨、骨和脂肪的干细胞)死亡。结果是死亡组织脱矿质或被新的但较弱的骨组织吸收(小梁变薄),随后导致软骨下骨折和股骨头塌陷。
其他提出的股骨头坏死(ON)发病机制包括由过量糖皮质激素影响骨和静脉内皮细胞的不利影响引起的血管收缩引起的变化,以及过量糖皮质激素相关的股骨头坏死(ON)涉及循环脂质的变化,可能会在供应骨的动脉中引起微栓子。
髋关节股骨头骨坏死的病因
创伤性和非创伤性因素的结合可直接导致股骨头骨坏死。在纵向队列研究和荟萃分析的基础上,发现了在股骨头坏死(ON)发展中起明确病因作用的直接危险因素。然而,相关风险因素是与股骨头坏死(ON)最终进展(直接)相关的大部分因素。
股骨头坏死(ON)的外伤原因
股骨头坏死(ON)的创伤性原因包括股骨颈骨折或脱位以及骨髓成分的直接损伤(例如与放射损伤、气压失调或沉箱病相关)。
股骨颈骨折或脱位的机制是骨外血管受损,导致髋关节受影响区域的血液供应中断。髋关节脱位是另一种类型的创伤性损伤,影响约20%的创伤相关股骨头坏死(ON)患者。
沉箱病(例如潜水减压)会导致氮气气泡的形成,从而阻塞小动脉,导致股骨头坏死(ON)。出现症状的患者可能会在经历此过程数年后出现髋关节股骨头坏死(ON)。压力的深度和持续时间以及暴露的次数是这种疾病进展的重要因素。
股骨头坏死(ON)的非外伤原因
许多研究报告称,长期使用皮质类固醇激素与股骨头坏死(ON)的发生相关,可能与药物的持续时间和总剂量直接相关。长期使用高剂量糖皮质激素治疗的患者似乎处于发生股骨头坏死(ON)的最大风险;然而,这些患者通常有多种其他危险因素。
接受长期治疗的患者中有9%至40%会发生糖皮质激素诱发的股骨头坏死(ON),而接受短期治疗的患者则发生率要低得多。一项荟萃分析和系统评价发现,近7%的患者发生股骨头坏死(ON)使用 < 2 g 皮质类固醇激素。根据这项荟萃分析,接受泼尼松剂量低于15 mg/d至20 mg/d治疗的患者发生股骨头坏死(ON)的风险较低。一项针对98,390名患者的基于人群的研究表明接受单次短期、低剂量甲强龙逐渐减量治疗的患者股骨头坏死(ON)的发生率为0.13%,而未接受甲强龙逐渐减量治疗的患者的股骨头坏死(ON)发生率为0.08%。
约31%的股骨头坏死(ON)患者与饮酒有关。与股骨头坏死(ON)相关的过量饮酒被认为是由于脂质形成过多和细胞内脂质沉积增加导致骨生成减少所致,导致骨细胞死亡和股骨头坏死(ON)。
高剂量皮质类固醇激素和过量饮酒共同构成了髋关节股骨头坏死(ON)发展的最高相关直接危险因素,并且占与创伤无关的病例的80%以上。一项研究比较了112名患有特发性髋关节股骨头坏死(ON)患者与168名对照者(没有全身性皮质类固醇激素使用史),与对照者相比,经常饮酒者的风险升高,并且与酒精存在明显的剂量反应关系。对于当前饮酒量低于400毫升/周、400毫升/周至1000毫升/周和超过1000 毫升/周的消费者来说,相对风险分别为3.3、9.8和17.9。
股骨头坏死(ON)在镰状细胞病患者中很常见,因为它容易导致红细胞镰状化和骨髓增生。大约50%的受影响患者在35岁时出现股骨头坏死(ON)。镰状细胞血红蛋白病可直接导致血管阻塞和股骨头坏死(ON)。
据报道,3%至30%的系统性红斑狼疮SLE患者会发生股骨头坏死(ON),最危险的是服用糖皮质激素和常规剂量泼尼松剂量大于20 mg/d的患者。据报道,高达60%的戈谢病(一种遗传性疾病)患者患有股骨头坏死(ON),因为它能够直接阻碍血管供应。戈谢病是一种常染色体隐性遗传代谢疾病,其中一种脂肪(脂质)称为葡萄糖脑苷脂不能被充分降解。通常情况下,身体会产生一种称为葡萄糖脑苷脂酶(细胞膜的正常部分)的酶,它会分解并回收葡萄糖脑苷脂。其他不太常见但与股骨头坏死(ON)明显相关的患者包括抗磷脂抗体、库欣病和系统性红斑狼疮SLE患者。急性淋巴细胞白血病、慢性粒细胞白血病和急性粒细胞淋巴瘤的发展,使患者因使用类固醇激素治疗这些疾病而面临更高的股骨头坏死(ON)风险。
胰腺炎(通常与使用皮质类固醇激素有关)、怀孕、化疗、吸烟、血管炎、胸膜炎和中枢神经系统因素,例如导致交感神经纤维数量减少的炎症反应(如类风湿性关节炎、克罗恩病)、夏科足和炎症性肠病),与股骨头坏死(ON)相关。
有一些证据表明股骨头坏死(ON)可能具有相关风险因素的遗传基础。例如,当过度饮酒是相关风险因素时,男性受到的影响是女性的3倍。然而,当狼疮或皮质类固醇激素的使用成为相关危险因素时,女性比男性更容易受到影响。系统性红斑狼疮SLE在女性中的发病率大约是男性的9倍。这种易感性增加是可能的,至少部分原因是与激素和性染色体有关的差异。血液透析、高尿酸患者的慢性肾衰竭或终末期肾病、贫血/痛风、HIV感染、高脂血症、器官移植和血管内凝血也与股骨头坏死(ON)的发生有关。尽管存在许多可能的关联和联系,但估计20%的股骨头坏死(ON)病例被标记为特发性或病因不明。
髋关节股骨头骨坏死的临床表现
髋关节疼痛是股骨头坏死(ON)晚期最常见的症状,尽管一小部分患者可能没有症状。腹股沟疼痛是最常见的症状,其次是大腿和臀部疼痛。疼痛可能因负重或关节运动而出现。大约三分之二的股骨头坏死(ON)患者会出现休息时疼痛,大约三分之一的患者会出现夜间疼痛。身体多个部位的疼痛很少见,表明存在多灶性过程。髋关节股骨头坏死(ON)的体格表现通常是非特异性的,但可能会导致受影响关节的活动范围减小、行走疼痛、Trendelenburg征和/或骨摩擦音。
髋关节股骨头骨坏死的临床评估
髋关节股骨头坏死(ON)通常通过:1)回顾患者病史,2)获得适当的放射学评估,3)确定病情阶段,以及4)制定治疗方案来解决。在评估患者是否患有股骨头坏死(ON),问题应针对评估疼痛史、药物使用(尤其是皮质类固醇)、手术、怀孕、创伤、慢性疾病(尤其是镰状细胞病、戈谢病、自身免疫性疾病和白血病)、吸烟和/或饮酒。当询问受伤/疾病时,重要的是要仔细探讨与髋部骨折、脱位或沉箱病相关的伤害,因为沉箱病是非创伤性的。
髋关节股骨头骨坏死的诊断和分类
在疾病的初始阶段诊断髋关节股骨头骨坏死对于治疗很重要;在初始阶段,疾病可能不会进展。大多数情况下,早期股骨头坏死(ON)患者一般没有症状,是偶然发现的;不幸的是,大多数患者直到股骨头坏死(ON)发展到后期才前来接受评估。尽管目前还没有已知的明确治疗方法可以永久阻止股骨头坏死(ON)进展到后期,但目前有一些治疗方法用于此目的,例如降脂剂、抗凝剂和双磷酸盐。
当患者出现症状、影像学检查结果一致、并且其他引起疼痛和骨异常的原因不太可能或已被排除时,就可以准确地做出股骨头坏死(ON)的诊断。除了临床和体检之外,放射线照片和磁共振成像(MRI)扫描等成像技术也用于诊断。首先,进行普通放射线照相评估,然后进行MRI。据报道,MRI对于检测早期股骨头坏死(ON)的特异性和敏感性<99%。MRI图像还可以通过对异常骨占据的股骨头区域进行数字化,定量评估病变的大小或受影响骨的受累程度。MRI变化包括T1加权图像上界限分明且均匀的局灶性病变,具有分隔正常骨和缺血骨的单密度线,以及T2加权图像上的第二条高强度线(特征性双线征标志)代表血管丰富的肉芽组织。这种级别的成像细节非常有用,因为受影响骨骼病变的大小和范围很重要,可以帮助指导治疗。然而,对于终末期疾病,股骨头坏死(ON)患者可能没有必要使用MRI,因为此阶段的治疗选择可能有限。
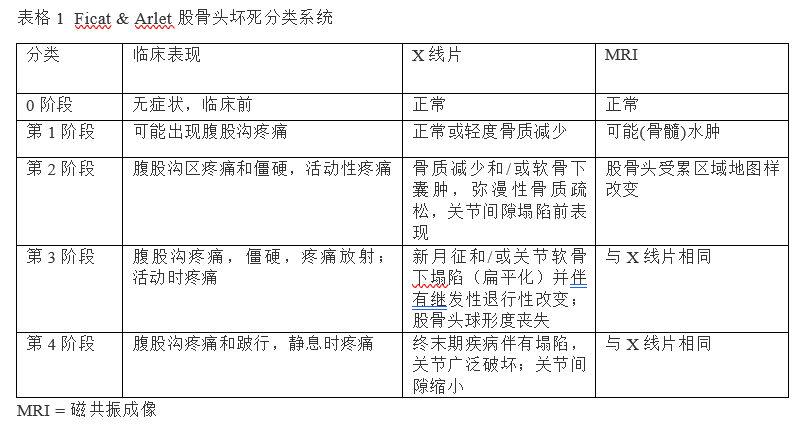
这些发现通常使用4个阶段的Ficat和Arlet系统进行分类,如此处和表1中所述。X线片可以在腹股沟疼痛等症状出现后数月内保持正常(第一阶段)。最早的放射学检查结果通常是轻微的骨密度变化,然后是硬化和囊性变(第二阶段)。然后,检查结果会从软骨下骨塌陷(第III期)发展到特征性新月征(在股骨头近端前外侧看到软骨下射线可透性),并随后出现股骨头球形度丧失(测量圆度)或股骨头最终关节塌陷,可见髋臼空间变窄和退行性变化(第四阶段)。要寻找的关键放射学特征包括1)阶段(塌陷前与塌陷后)、2)病变大小和3)股骨头凹陷程度。

右侧股骨头坏死的X线片表现:双线征,承重区域塌陷
右侧股骨头坏死的X线片表现:双线征,承重区
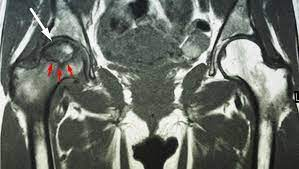
右侧股骨头坏死的核磁共振MRI平扫表现:新月征
右侧髋关节股骨头坏死X线片(上图)及MRI表现(下图)
生成骨骼三维图像的计算机断层扫描具有中等敏感性,但不具有特异性,可能会给患者带来显着的辐射负担。如果股骨头已经塌陷,计算机断层扫描可能具有一定的特异性。幸运的是,大多数临床医生无需计算机断层扫描即可诊断出股骨头骨坏死,而计算机断层扫描通常用于区分塌陷前和塌陷后疾病。
髋关节股骨头骨坏死的鉴别诊断
由于有症状的髋关节股骨头坏死(ON)患者可能会出现与许多其他髋关节病变类似的症状,因此在最终诊断之前应充分排除这些症状。骨髓水肿综合征和软骨下骨折是也需要考虑的许多潜在诊断中的两个。
与骨坏死相关的病因
创伤相关的危险因素
股骨颈骨折
脱位或骨折脱位
镰状细胞性贫血症
血红蛋白病
沉箱病(气压失调)
戈谢病
辐射
非创伤相关的危险因素
皮质类固醇激素
饮酒
系统性红斑狼疮
库欣病
皮质醇分泌过多(罕见)
慢性肾功能衰竭/血液透析
胰腺炎
妊娠
高脂血症
器官移植
血管内凝血
血栓性静脉炎
吸烟
高尿酸血症/痛风
艾滋病病毒感染
其他潜在风险因素
特发性原因
骨髓水肿综合征,也称为髋部暂时性骨质减少,可能单独发生或与损伤相关,特别是那些导致神经损伤的创伤。在后一种情况下,慢性疼痛和短暂性骨质减少是复杂区域疼痛综合征(也称为反射性交感神经营养不良、灼痛等术语)的特征。骨髓水肿综合征可根据组织学和MRI与股骨头坏死(ON)相鉴别。
股骨头软骨下骨折通常发生在已有骨质减少的患者中,通常被认为代表不全骨折。这些骨折可能很难通过平片观察到。早期病变有时会出现轻微的扁平化;股骨头塌陷是进行性的。
髋关节股骨头骨坏死的临床治疗
在制定针对症状性髋关节骨关节炎的最佳治疗方法时要考虑的因素应旨在治疗骨关节炎的分期和受累程度、骨受累的程度和位置、症状的存在(或不存在)以及患者的合并症。治疗的目标是尽可能长时间地保留天然髋关节,同时考虑患者年龄、活动能力、职业和生活方式等生活质量问题。处理髋关节股骨头坏死(ON)的三种主要治疗选择包括 1)非手术治疗、2)关节保留手术和 3)全髋关节置换术THA。
非创伤性原因引起的髋关节股骨头坏死(ON)的影响引起了特别关注。对于受影响的患者,67%的人报告没有任何症状,但最终可能会出现关节塌陷。无症状的中等、尤其是大面积股骨头骨坏死的自然病程是病情恶化,最终发展为终末期疾病,许多患者出现股骨头塌陷。对于有症状的患者,大约80%至85%的病例会在2年内导致股骨头塌陷。因此,早期诊断股骨头坏死(ON)可能会提供早期治疗的机会,这可以防止塌陷,并最终避免股骨头塌陷而需要进行的全髋关节置换的手术治疗。然而,大多数患者在病程晚期就诊,对于那些已知或可能存在危险因素的患者,特别是使用大剂量皮质类固醇激素的患者,必须高度怀疑(存在股骨头坏死(ON))。
同样,对于无症状的股骨头坏死(ON)患者,应考虑影响股骨头坏死病变的大小、范围和位置。一般来说,影响股骨头15%以下的病变最好采用非手术治疗;15%至30%之间的病变应进行手术治疗;尽管进行了手术干预,但涉及超过30%股骨头的病变仍可能进展至塌陷,并最终需要全髋关节置换术THA。
髋关节股骨头骨坏死的非手术治疗选择
物理治疗
物理治疗可以缓解和减轻一些症状,但通常不会阻止进行性髋关节骨性关节炎进展到后期。同样,使用拐杖或手杖等辅助装置限制负重可能有助于控制疼痛、虚弱和痛性步态等症状。如果治疗的目标是防止髋关节需要全髋关节置换,那么物理治疗是不合适的,并且迄今为止没有证据表明负重限制有助于防止进行性骨关节炎疾病进展为终末期疾病。
药物
非甾体类抗炎药和对乙酰氨基酚可以暂时缓解有症状患者的疼痛。当其他药物无法有效控制中度至重度疼痛时,在考虑手术选择时,可以明智地短期使用阿片类药物。
目前正在使用但未经证实或可靠地用于治疗股骨头坏死(ON)的研究药物选择包括 1)抗凝剂、2)双膦酸盐抗吸收剂、3)降胆固醇他汀类药物和 4)高压氧。
早期股骨头坏死(ON)的手术选择
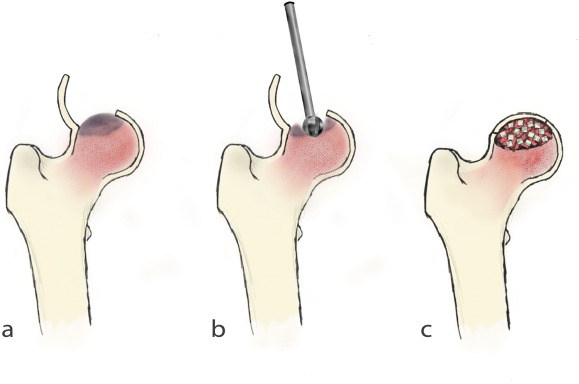
髓心减压
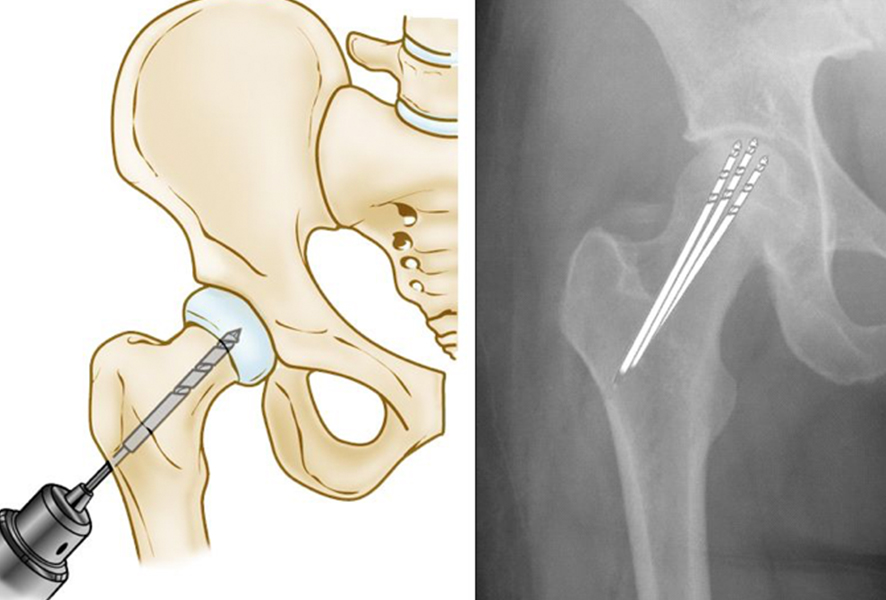
股骨头坏死的髓芯减压术
髓心减压是一种微创手术技术,用于控制病情早期(塌陷前)的症状(例如Ficat和Arlet I期和II期)。该手术包括在股骨头上钻孔以缓解压力并为新血管创造通道以滋养受影响的区域。已发表的髓心减压成功率差异很大,从40%到100%不等,具体取决于患者群体。髓心减压后的成功率在最早疾病阶段的患者中可见。成功进行髓心减压手术的患者通常会在几个月后恢复独立行走,并且可以完全缓解疼痛。
骨移植
髓心减压可以与骨移植相结合,帮助再生健康的骨骼并支撑髋关节的软骨。骨移植物是移植到坏死或死骨区域的健康骨组织。一种标准技术使用自体移植,涉及从身体的一个部位取出骨头并将其移动到身体的另一部位。从捐赠者或尸体上采集的骨移植物称为同种异体移植物,通常通过骨库获取。
骨髓抽吸浓缩物
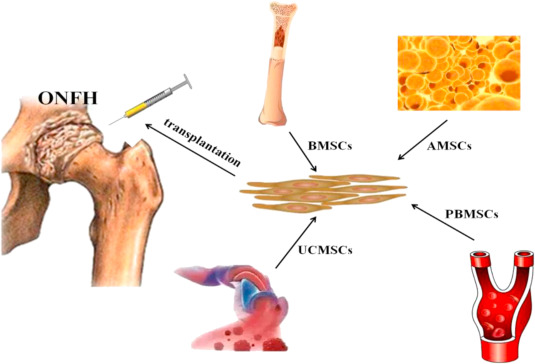
干细胞技术治疗股骨头坏死
髓心减压配合骨髓抽吸浓缩物注射是使用浓缩骨髓,将其注射到股骨头坏死的死骨中。这项研究技术从患者的骨髓中采集干细胞并将其注射到股骨头坏死(ON)区域。骨髓抽吸浓缩被认为可以防止疾病进一步发展并刺激新骨生长。
经皮钻孔
另一种手术选择是经皮钻孔。在此过程中,通过股骨颈经皮钻一个孔,到达股骨头的受影响部位。 一份对45个髋关节进行平均随访24个月的报告显示,30个患有Ficat 和 Arlet I期疾病的髋关节中有24 个(80%)取得了成功的结果(定义为 Harris 髋关节评分 < 70)。一项最近的研究比较了多个钻探与标准髓心减压相比,显示经皮钻探获得更好的结果。
晚期股骨头坏死(ON)的手术选择
血管化骨移植
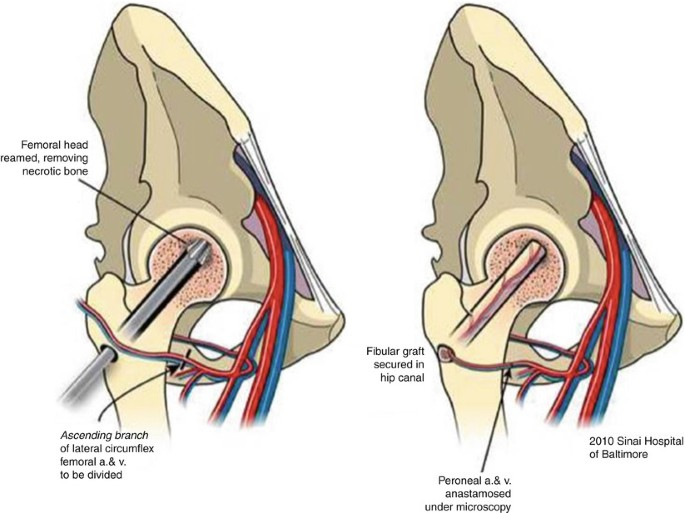
带血管蒂的髂骨或腓骨移植术,治疗股骨头坏死
血管化腓骨移植是一种更为复杂的外科手术,其中从腓骨及其血液供应中取出一段骨。然后将移植物移植到股骨颈和股骨头上形成的孔道中,并重新连接动脉和静脉以帮助愈合股骨头坏死(ON)。
截骨术
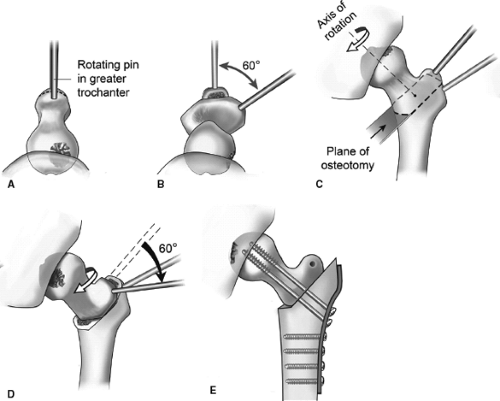
股骨近段旋转截骨术治疗股骨头坏死
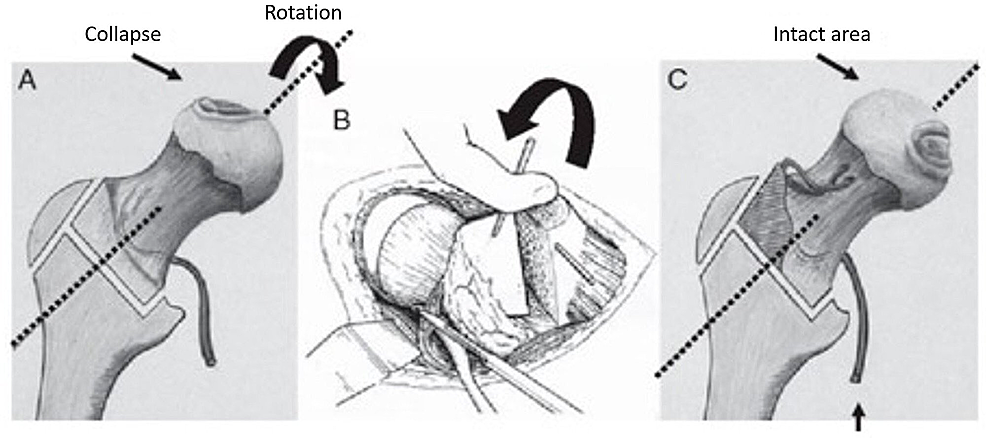
股骨近段旋转截骨术治疗股骨头坏死
股骨近段旋转截骨术治疗股骨头坏死
髋关节截骨术可以将坏死骨从主要承重区域去除。尽管该手术可能会延迟THA手术,对于股骨头轻度塌陷前或早期塌陷后的股骨头坏死患者最有用。然而,截骨术的一个结果是使得未来可能的全髋关节置换术更具挑战性,并且通常与骨不连的风险增加有关。
非血管化骨移植
非血管化骨移植手术有3种类型:1) 活板门手术、2) 灯泡技术和 3) Phemister 技术。
活板门手术
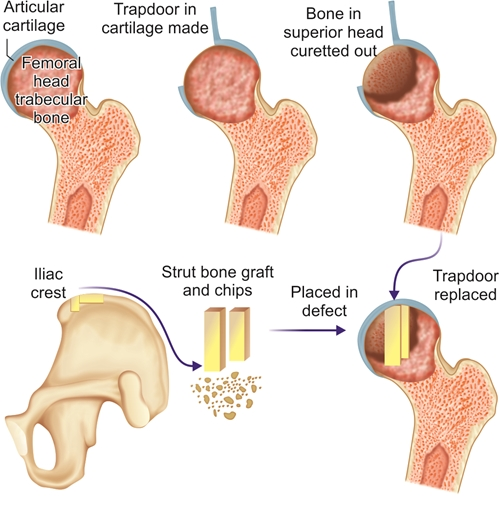
一种自体松质骨和皮质骨移植术,已成功用于Ficat 和 Arlet III期髋关节股骨头坏死(ON)的中小型病变患者。对23名Ficat和Arlet III期或 IV期股骨头坏死(ON)患者进行的30次(在股骨头上制作的)活板门手术的结果显示,根据Harris评分系统的判定,结果均良好或极好。
灯泡技术
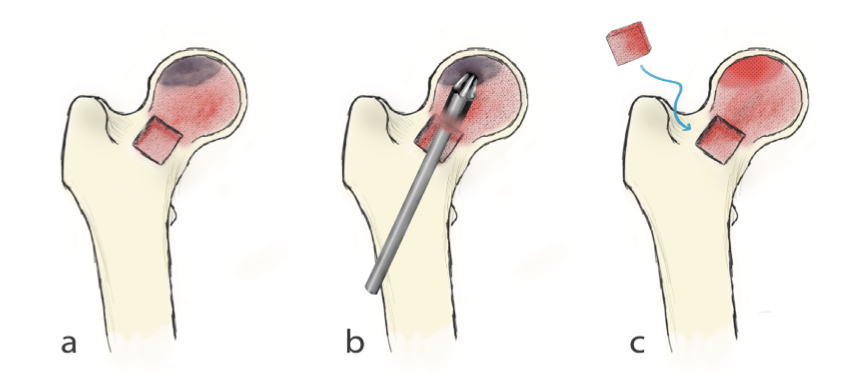
灯泡技术使用股骨颈前部的皮质窗口。可以使用该窗口去除坏死骨,随后可以用非血管化骨移植物填充。Wang 等对110名接受灯泡手术的患者(138髋)进行了评估。在平均25个月的随访中,平均Harris髋关节评分从62分提高到79分。在最近的随访中,总共94个髋关节(68%)被认为取得了成功。ARCO分期IIa期患者中100%、IIb期患者中77%、IIc和IIIa期患者中51%出现放射学改善。
Phemister技术
在Phemister技术中,通过股骨颈插入环钻以形成通向病变部位的管道。然后插入第二个环钻以形成通往病变部位的另一条管道。然后可以将皮质支柱移植物放置在病变处。最近的一项评论报告称,该手术的临床成功率在36%至90%之间。
全髋关节置换术(THA)
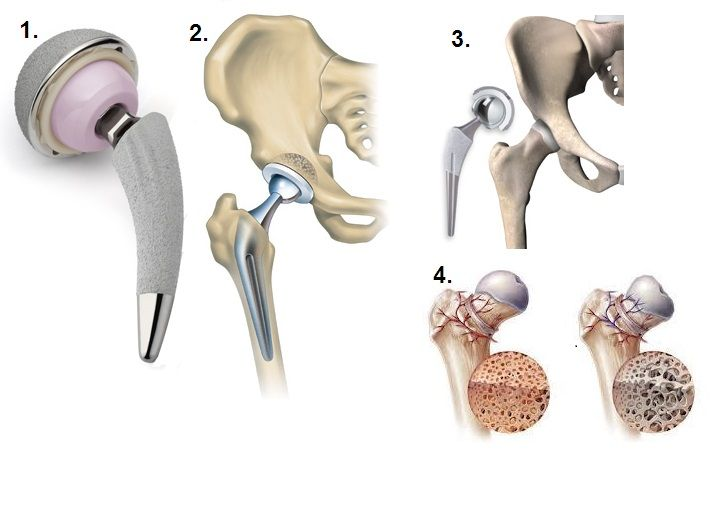
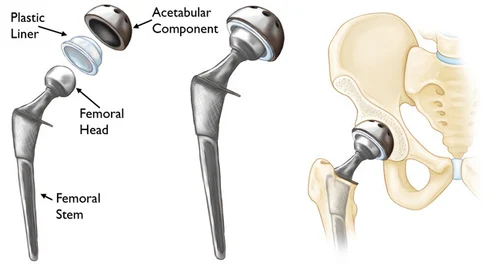
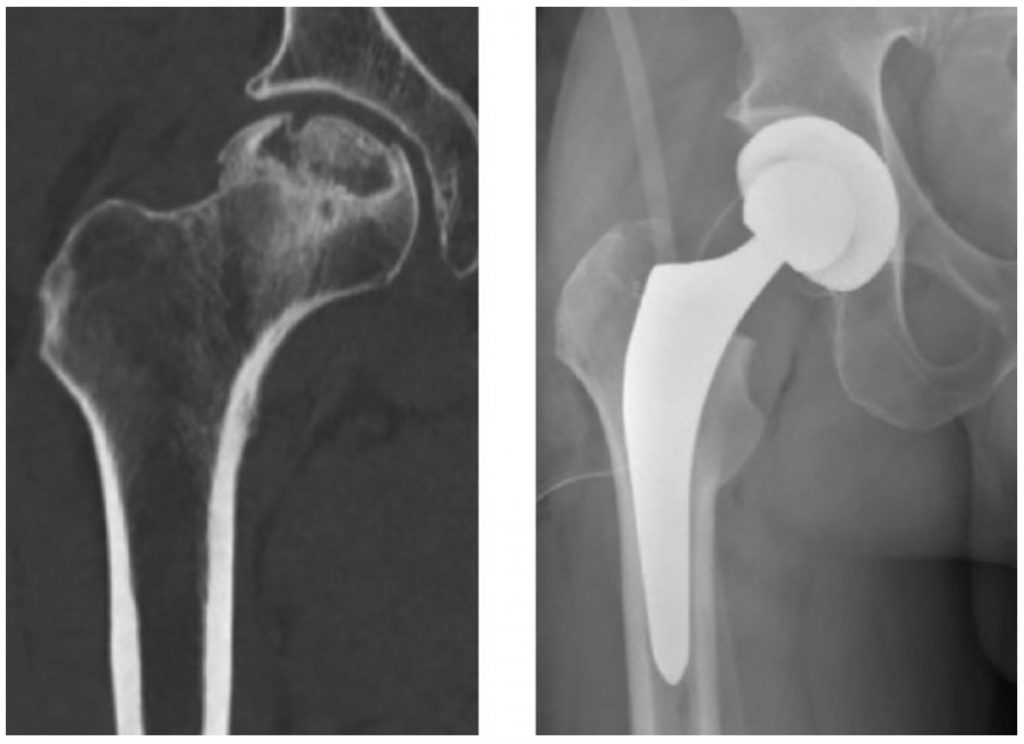
一旦股骨头发生严重塌陷,置换髋关节是唯一实用的手术选择,并且可以在晚期股骨头坏死中提供最可预测的疼痛缓解。全髋关节置换术(THA)成功地缓解了大多数患者的疼痛并恢复了功能。在全髋关节置换术(THA)中,构成髋关节的患病软骨和骨骼被由金属和塑料制成的人工关节假体取代。人工髋关节置换术通常可以使用15年,然后就会磨损并需要修复。对于较年轻的患者,由于可能存在活动限制,全髋关节置换术(THA)可能不是最佳解决方案。此外,由于假肢有使用寿命限制(长期使用后部件会磨损),这些患者可能需要在以后的生活中进行全髋关节置换术(THA)翻修。必须仔细考虑全髋关节置换术并与生活质量问题进行权衡,但年轻患者并非绝对禁忌。
关于髋关节股骨头坏死(ON)的患者教育
预防股骨头坏死(ON)
对患者进行有关危险因素、治疗和管理的教育对于患者对其病情做出更明智的决定至关重要。股骨头坏死(ON)教育过程涉及识别个人的相关疾病和与股骨头坏死(ON)相关的危险因素。
无症状股骨头坏死的患者进展为有症状疾病和股骨头塌陷的可能性很高。对无症状疾病患者的教育是预防性的,也是必要的,以确保改变危险因素和优化护理。预防非创伤性股骨头坏死(ON)需要:1)避免过量饮酒,定义为男性每周< 15杯饮酒,女性每周< 8 杯饮酒,2)避免吸烟,以及 3)将皮质类固醇激素减少到尽可能低的治疗剂量。告知患者皮质类固醇激素的使用与股骨头坏死(ON)潜在发展之间的相关性对于治疗这种疾病至关重要。
预防股骨头坏死(ON)的进展
应告知诊断为早期骨关节炎的患者采取上述预防措施,并应避免对关节施加过度压力,遵循健康饮食,并保持适当的体重以减缓骨关节炎的进展。尽管健康饮食本身并不能直接减少患者关节的压力,但减肥(如果超重/肥胖)会减少髋关节的轴向负荷,从而减少施加到股骨头/颈(股骨头和股骨颈)的压力。
结论
股骨头坏死(ON)是一种病理性的、经常引起疼痛的病症,涉及组织坏死区域,可影响身体的任何骨关节。髋关节是最常见的股骨头坏死(ON)部位,当最初诊断出股骨头坏死(ON)发生在身体的其他部位时,应始终利用放射线筛查和MRI扫描进行正确评估。越早诊断股骨头坏死,无需手术干预或采用微创手术技术来挽救髋关节的机会就越大。
做出股骨头坏死(ON)诊断后,将考虑病变的大小、范围和位置以及分类阶段,以制定最佳的治疗计划。在此过程中,症状的存在或不存在很重要。治疗的目标包括尝试尽可能长时间地保留天然髋关节,并考虑患者的生活方式和生活质量问题。迄今为止,治疗股骨头坏死(ON)的两种主要治疗选择包括髋关节保留手术(保髋治疗)和全髋关节置换术THA。对患者进行有关潜在危险因素和股骨头坏死(ON)发展的教育,对于预防该病症和/或潜在地预防或阻止早期疾病进展为晚期疾病至关重要。
Osteonecrosis of the Hip: A Primer
Abstract
In this report, we deliver a concise and up-to-date review of osteonecrosis, a pathologic, painful, and often disabling condition that is believed to result from the temporary or permanent disruption of blood supply to an affected area of bone. We will discuss the epidemiology (disease distribution), pathogenesis (mechanism of development), etiology (associated risk factors, causes, and disorders), clinical manifestations (reported symptoms and physical findings), diagnosis and classification, and treatment options for hip osteonecrosis.
文献出处:Michelle J Lespasio, Nipun Sodhi, Michael A Mont. Osteonecrosis of the Hip: A Primer. Review Perm J. 2019;23:18-100. doi: 10.7812/TPP/18-100.
INTRODUCTION
The intent of this article is to present an update on osteonecrosis (ON) affecting the femoral head or hip joint and how it can best be managed in the adult population. Specifically, this report will encompass the epidemiology, pathogenesis, etiology, clinical manifestations, diagnosis and classification, and treatment options for hip ON. ON, also referred to as avascular necrosis, aseptic necrosis, or ischemic bone necrosis, is associated with many disorders and risk factors that cause mature bone cells to die, leading to bone destruction (eg, collapse) or end-stage arthritis of the femoral head. The condition can occur in any bone in the body (eg, upper extremity, knees, shoulders, and ankles), or in more than 1 bone at different times, but it most commonly affects the hip joint. When initially diagnosed in an area other than the hip, the hip should simultaneously be evaluated clinically and with radiographic and other imaging studies. The causes of ON are classified as either traumatic (related to an injury) or atraumatic (not related to an injury). Accurately diagnosing and classifying ON are important in helping to direct treatment options. Identification of associated risk factors and patient education are important in successful management of ON. Targeting associated risk factors, pharmacologic management, and/or surgery, including joint preserving procedures and total hip arthroplasty (THA), also play significant roles in the clinical care of patients with ON.
EPIDEMIOLOGY OF HIP OSTEONECROSIS
Although the exact prevalence of ON is unknown, the incidence is estimated to be between 20,000 to 30,000 newly diagnosed patients each year in the US.1 ON is the underlying diagnosis in approximately 10% of all THA in the US.2,3 ON affects people of all ages, although it is most commonly seen in patients between the ages of 30 and 65 years.4 The mean age at diagnosis is typically younger than age 50 years.3 The male-to-female ratio varies depending on the associated comorbidities. For example, alcohol-associated ON is more common in men, whereas ON associated with systemic lupus erythematosus (SLE) is more common in women.3
More than 20,000 people each year require hospital treatment for hip ON.4 In many of these cases, both hips are affected by the condition. Most commonly, ON affects the proximal end (epiphysis) of the femur (hip bone).
PATHOGENESIS OF HIP OSTEONECROSIS
The mechanism(s) by which hip ON develops remains unclear. For the most part, hip ON is believed to result from the combined effects of genetic predisposition, metabolic factors, and local factors affecting blood supply including vascular damage, increased intraosseous pressure, and mechanical stresses.2,5,6 Most experts agree that a lack of blood supply to the femoral head and bone marrow, which produces stem cells and platelets, causes death of the osteocytes (cells within mature bone) and/or mesenchymal cells (stem cells that form cartilage, bone, and fat).7 The result is demineralization or resorption of the dead tissue by new but weaker osseous tissue (trabecular thinning), subsequently leading to subchondral fracture and collapse of the femoral head.
Other proposed mechanisms for the pathogenesis of ON include vasoconstriction-induced changes caused by the adverse effects of excess glucocorticosteroids affecting bone and venous endothelial cells8,9 and excess glucocorticoid-associated ON involving alterations in circulating lipids believed to cause microemboli in the arteries that supply bone with blood.10
ETIOLOGY OF HIP OSTEONECROSIS
A combination of traumatic and atraumatic factors can directly contribute to the etiology of ON (see Sidebar: Etiologic Factors Associated with Osteonecrosis). On the basis of longitudinal cohort studies and meta-analyses, direct risk factors have been discovered that play a definitive etiologic role in the development of ON. Associated risk factors, however, account for most of the links to the eventual development of ON.11
Traumatic Causes of Hip Osteonecrosis
Traumatic causes of ON include femoral neck fractures or dislocations as well as direct injury of bone of marrow elements (eg, related to radiation injury, dysbarism, or Caisson disease). The mechanism involved in femoral neck fractures or dislocations is damage to the extraosseous blood vessels, which results in disrupted blood supply to the affected region of the hip. Hip dislocation is another type of traumatic injury, which affects approximately 20% of trauma-related ON patients.12
Caisson disease (eg, decompression in scuba diving) causes the formation of nitrogen bubbles that can occlude arterioles, leading to ON. Patients who develop symptoms can develop hip ON years after exposure to this process. The depth and duration of pressure and number of exposures are important factors in the progression of this disorder.13
Atraumatic Causes of Hip Osteonecrosis
Numerous studies report prolonged use of corticosteroids associated with the development of ON can be directly related to duration and total dosage of the medication.14–16 Patients treated with prolonged high doses of glucocorticoids appear to be at the greatest risk of developing ON; however, these patients often have multiple other risk factors.
Glucocorticoid-induced ON develops in 9% to 40% of patients receiving long-term therapy, and develops much less frequently in patients receiving short-term therapy.17 One meta-analysis and systematic review identified an incidence of ON in nearly 7% of patients who used < 2 g of corticosteroids.18 From this meta-analysis, a lower risk was seen in patients treated with doses of prednisone less than 15 mg/d to 20 mg/d.18 One population-based study of 98,390 patients showed the incidence of hip ON among patients who had received a single short-term, low-dose methylprednisolone taper pack was 0.13%, compared with 0.08% in patients who were not prescribed a methylprednisolone taper pack, thus indicating a number needed to harm of 2041 patients.19
Alcohol use has been associated with approximately 31% of patients who develop hip ON.3,20–22 Excessive alcohol consumption related to ON of the hip is believed to result from the decreased bone genesis caused by excess lipid formation and increased intracellular lipid deposits, leading to osteocyte death and ON.23
High doses of corticosteroids and excessive alcohol use together present the highest associated direct risk factors for the development of hip ON24 and account for more than 80% of cases not related to trauma.3,6 One study compared 112 patients who had idiopathic hip ON and no history of systemic corticosteroid use with 168 controls.3,20 An elevated risk for regular alcohol drinkers and a clear dose-response relationship with alcohol were noted, compared with controls. The relative risks were 3.3, 9.8, and 17.9 for current consumers of less than 400 mL/wk, 400 mL/wk to 1000 mL/wk, and more than 1000 mL/wk of alcohol, respectively.9
ON is common in patients with sickle cell disease because of its propensity to cause red blood cell sickling and bone marrow hyperplasia. Approximately 50% of affected patients develop ON by the age of 35 years.25 Sickle cell hemoglobinopathy can directly cause vascular obstruction and ON.
The development of ON has been reported in 3% to 30% of patients with SLE, and those most at risk are patients who have taken glucocorticoids with regular doses of prednisone greater than 20 mg/d.3,26–28 ON has been reported in as many as 60% of patients with Gaucher disease (a hereditary disorder) because of its ability to directly obstruct vascular supply.3,29,30 Gaucher disease is an autosomal recessive inherited disorder of metabolism where a type of fat (lipid) called glucocerebroside cannot be adequately degraded. Normally, the body makes an enzyme called glucocerebrosidase (a normal part of the cell membrane) that breaks down and recycles glucocerebroside.31
Other less common but apparent links to hip ON include patients with antiphospholipid antibodies, Cushing disease,29 and SLE. The development of acute lymphoblastic leukemia, chronic myeloid leukemia, and acute myeloid lymphoma3,32 places patients at increased risk for ON related to the treatment with steroids for these conditions.
Pancreatitis (usually associated with use of corticosteroids), pregnancy, chemotherapy, smoking, vasculitis, pleuritis, and central nervous system factors such as an inflammatory response resulting in a reduction in the number of sympathetic nerve fibers (as seen in rheumatoid arthritis, Crohn disease, Charcot foot, and inflammatory bowel disease), have been associated with ON.33
There is some evidence that hip ON may have a genetic basis underlying associated risk factors.34 For example, men are affected as much as 3 times more than women when excessive alcohol use is the associated risk factor. However, when lupus or corticosteroid use are the associated risk factors, women are affected more often than men.26,27,32 SLE is approximately 9 times more common in women than in men.35 This increased susceptibility may be made possible, at least in part, owing to differences related to hormones and sex chromosomes.35 Chronic renal failure or end-stage renal disease in patients on hemodialysis, hyperuricemia/gout, HIV infection, hyperlipidemia, organ transplantation, and intravascular coagulation are also linked to the development of ON.31,32,36–39 Despite the many possible associations and links, an estimated 20% of ON cases are labeled as idiopathic or of unknown etiology.7
CLINICAL MANIFESTATIONS OF HIP OSTEONECROSIS
Hip pain is the most commonly reported symptom of later-stage ON, although a small proportion of patients may not have symptoms. Pain in the groin is the most commonly reported symptom, followed by pain referred into the thigh and buttock. Pain can present with weightbearing or joint motion. Pain at rest occurs in approximately two-thirds of patients with ON, and pain at night occurs in approximately one-third of patients.33 Pain in multiple locations of the body is rare and suggests a multifocal process. Physical findings of hip ON are generally nonspecific but may entail reduced range of motion of the affected joint, painful ambulation, Trendelenburg sign, and/or crepitus.3,40,41
Clinical Assessment of Hip Osteonecrosis
ON of the hip is generally addressed by 1) review of a patient’s medical history, 2) obtaining appropriate radiologic evaluation, 3) determining the stage of the condition, and 4) developing a plan for treatment options.42,43 When evaluating a patient for ON, questions should be directed at assessing a history of pain, use of medications (especially corticosteroids), surgery, pregnancy, trauma, chronic medical conditions (especially sickle cell disease, Gaucher disease, autoimmune disease, and leukemia), smoking, and/or alcohol use. When asking about injuries/illnesses, it is important to carefully explore injuries related to hip fractures, dislocations, or scuba diving because Caisson disease is atraumatic.
DIAGNOSIS AND CLASSIFICATION OF HIP OSTEONECROSIS
Diagnosing hip ON in the initial stages of the disorder is important for management43–46; at initial stages, the disease may not progress. In most cases, patients with early-stage ON are generally without symptoms and are identified incidentally; unfortunately, most patients do not present for evaluation until the ON has reached later stages. Although there is presently no definitive treatment known to permanently halt ON from progressing to later stages, there are treatment methods, such as lipid lowering agents, anticoagulants, and bisphosphonates, currently being used for this purpose.36–38
A diagnosis of ON can accurately be made when a patient is symptomatic, imaging findings are compatible, and other causes of pain and bony abnormalities either are unlikely or have been excluded. Beyond the clinical and physical examination, imaging techniques such as radiographs and magnetic resonance imaging (MRI) scanning are also used for diagnosis. Plain radiographic evaluation is performed first, followed by MRI. MRI has been reported to be < 99% specific and sensitive for detecting early ON.47,48 MRI images can also quantitatively assess the size of the lesion or involvement of the affected bone by digitizing the area of the femoral head occupied by bone with abnormal texture.49 MRI changes include well-demarcated and homogeneous focal lesions on T1-weighted images with a single-density line separating normal and ischemic bone, as well as a second high-intensity line on T2-weighted images (the pathognomonic double-line sign) representing hypervascular granulation tissue.3 This level of imaging detail is useful because the size and extent of the lesion of the affected bone is important and can help direct treatment. For end-stage disease, however, use of MRI in patients with ON may be unnecessary because treatment options at this stage can be limited.
These findings are often classified using the 4-stage Ficat and Arlet system, which is described here and in Table 1. The plain radiograph can remain normal for months after the onset of symptoms such as groin pain (Stage I). The earliest radiographic findings are usually mild density changes, followed by sclerosis and cysts (Stage II). Findings then progress to the pathognomonic crescent sign (subchondral radiolucency seen in the anterolateral aspect of the proximal femoral head) from subchondral collapse (Stage III), and subsequent loss of sphericity (measurement of the roundness) or collapse of the femoral head with eventual joint-space narrowing and degenerative changes in the acetabulum that are visible (Stage IV). Key radiographic features to look for include 1) stage (precollapse vs postcollapse), 2) size of lesion, and 3) amount of head depression.
Table 1
Ficat & Arlet classification system of the femoral head
Classification Clinical Radiographs MRI
Stage 0 No symptoms; preclinical Normal Normal
Stage 1 Possible groin pain Normal or mild osteopenia Possible edema
Stage 2 Groin pain and stiffness; pain with activity Osteopenia and/or subchondral cysts; diffuse porosis; precollapse of joint space Outlines area of involvement of the femoral head
Stage 3 Groin pain, stiffness, radiation of pain; pain with activity Crescent sign and/or subchondral collapse (flattening) of joint with secondary degenerative changes; loss of sphericity of femoral head Same as radiographs
Stage 4 Groin pain and limp; pain at rest End-stage disease with collapse; extensive destruction of joint; reduced joint space Same as radiographs
Open in a separate window
MRI = magnetic resonance imaging
A computed tomography scan producing a 3-dimensional picture of the bone has moderate sensitivity but is nonspecific and can pose a significant radiation burden to patients. Computed tomography can have some specificity if there is already femoral head collapse. Fortunately, most clinicians are assured with their diagnosis of ON without computed tomography scanning, which is generally reserved for distinguishing precollapse and postcollapse disease.
Differential Diagnosis of Hip Osteonecrosis
Because patients with symptomatic hip ON can present with symptoms similar to many other hip pathologies, these should be adequately ruled out before final diagnosis. Bone marrow edema syndrome and subchondral fractures are two of many potential diagnoses that need to also be considered.
Etiologic Factors Associated with Osteonecrosis
Traumatic-associated risk factors
Femoral neck fracture
Dislocation or fracture-dislocation
Sickle cell disease
Hemoglobinopathies
Caisson disease (dysbarism)
Gaucher disease
Radiation
Atraumatic-associated risk factors
Corticosteroid administration
Alcohol use
Systemic lupus erthyematosus
Cushing disease
Hypersecretion of cortisol (rare)
Chronic renal failure/hemodialysis
Pancreatitis
Pregnancy
Hyperlipidemia
Organ transplantation
Intravascular coagulation
Thrombophlebitis
Cigarette smoking
Hyperuricemia/gout
HIV
Other potential risk factors
Idiopathic causes
Bone marrow edema syndrome, also known as transient osteopenia of the hip, may occur in isolation or in association with injuries, particularly those that result in neurologic damage. In the latter situation, chronic pain and transient osteopenia are features of the complex regional pain syndrome (also known as reflex sympathetic dystrophy, causalgia, and other terms).3 Bone marrow edema syndrome can be differentiated from ON on the basis of histologic and MRI findings.
Subchondral fracture of the femoral head typically occurs in patients with preexisting osteopenia and is generally thought to represent an insufficiency fracture.50 These fractures may be difficult to visualize with plain radiographs. Subtle flattening is sometimes present with early lesions; collapse of the femoral head is progressive.
CLINICAL MANAGEMENT OF HIP OSTEONECROSIS
Factors to consider when developing an optimal management approach for symptomatic ON of the hip should be aimed at treating the stage and degree of involvement of ON, the extent and location of bony involvement, the presence (or absence) of symptoms, and the patient’s comorbidities. The goal of therapy is to preserve the biological hip joint for as long as possible while also taking into consideration quality of life issues such as patient age, mobility, occupation, and lifestyle. Three main therapeutic options for management of hip ON include 1) nonoperative management, 2) joint-preserving procedures, and 3) THA.
The effects of atraumatic causes of hip ON pose special concerns. For those affected, 67% report no symptoms but may eventually go on to have a collapsed joint.51 The natural history of asymptomatic medium-sized, and especially large, osteonecrotic lesions is progression to worsening of the condition and eventually end-stage disease and collapse of the hip in a substantial number of patients. For those with symptoms, approximately 80% to 85% of cases will result in collapse of the femoral head within 2 years.6 Early diagnosis of ON may therefore provide the opportunity for early treatment, which can prevent collapse and, ultimately, the need for total joint arthroplasty. However, most patients present late in the course of the disease, and a high index of suspicion is necessary for those with known or probable risk factors, particularly patients with high-dose corticosteroid use.3
Similarly for patients with asymptomatic hip ON, the size, extent, and location of the necrotic lesion affecting the femoral head should be considered. Generally, lesions affecting less than 15% of the femoral head are best managed nonoperatively; lesions between 15% to 30% should be managed surgically; and lesions involving more than 30% of the femoral head are likely to progress to collapse, despite surgical intervention, and eventually require THA.3,52,53
Nonsurgical Treatment Options in Hip Osteonecrosis
Physical Therapy Physical therapy may provide relief and alleviate some symptoms but generally will not preclude progressive hip ON from advancing to later stages.54 Similarly, restricting weight-bearing with the use of assistive devices such as crutches or a cane may be useful to control symptoms of pain, weakness, and antalgic gait. Physical therapy is not appropriate if the goal of treatment is to prevent the hip from requiring THA, and to date there is no evidence that weight-bearing restrictions are helpful in preventing progressive ON disease from advancing to end-stage disease.
Medications Nonsteroidal anti-inflammatory drugs and acetaminophen may provide temporary relief of pain in symptomatic patients. Opioid medications may be used judiciously and for short periods of time when other agents are ineffective to manage moderate-to-severe pain while surgical options are being considered.
Investigational medication options currently being used but that are not proven or reliably used to treat ON include 1) anticoagulants, 2) bisphosphonate antiresorptive agents, 3) cholesterol lowering statins, and 4) hyperbaric oxygen.
Surgical Options in Early-Stage Hip Osteonecrosis
Core Decompression Core decompression is a minimally invasive surgical technique performed to manage symptoms in early stages (precollapse) of the condition (eg, Ficat and Arlet Stages I and II). The procedure involves drilling holes into the femoral head to relieve pressure and create channels for new blood vessels to nourish the affected areas. The published success rates of core decompression vary greatly from 40% to 100%, depending on patient population.35 Higher success rates after core decompression are seen in patients with the earliest disease stages. Patients with successful core decompression procedures typically return to unassisted ambulation after several months and can have complete pain relief.55
Bone Grafting Core decompression can be combined with bone grafting to help regenerate healthy bone and support cartilage at the hip joint. A bone graft is healthy bone tissue that is transplanted to the area of necrotic or dead bone. A standard technique uses an autograft that involves taking bone from one part of the body and moving it to another part of the body. A bone graft that is harvested from a donor or cadaver is called an allograft and is typically acquired through a bone bank.
Bone Marrow Aspirate Concentration The bone marrow aspirate concentration injection procedure with core decompression involves the use of concentrated bone marrow that is injected into the dead bone of the hip. This investigational technique harvests stem cells from a patient’s bone marrow and injects them into the area of ON.9 The bone marrow aspirate concentration procedure is hypothesized to prevent further progression of the disease and to stimulate new bone growth.56
Percutaneous Drilling Another surgical option is percutaneous drilling. In this procedure, a hole is drilled percutaneously through the femoral neck to the affected site in the femoral head. One report on 45 hips with a mean follow-up of 24 months reported 24 (80%) of 30 hips with Ficat and Arlet Stage I disease had successful outcomes (defined as Harris Hip Score < 70).57 A more recent study comparing multiple drilling vs standard core decompression showed favorable results in favor of percutanteous drilling.28
Surgical Options in Advanced-Stage Hip Osteonecrosis
Vascularized Bone Graft A vascularized fibula graft is a more involved surgical procedure in which a segment of bone is taken from the fibula with its blood supply. The graft is then transplanted into a hole created in the femoral neck and head, and the artery and vein are reattached to help heal the area of ON.55
Osteotomy Osteotomy in hip ON can be performed to remove necrotic bone away from primary weight-bearing areas. Although this operation may delay THA surgery, it is most useful in patients with idiopathic ON who demonstrate small precollapse or early postcollapse of the femoral head. A consequence of osteotomies, however, is that they make subsequent THA more challenging and are often associated with an increased risk of nonunion of the bone.
Nonvascularized Bone Graft There are 3 types of nonvascularized bone grafting surgeries: 1) trapdoor procedure, 2) lightbulb technique, and 3) Phemister technique. The trapdoor procedure is one in which autogenous cancellous and cortical bone grafting have been successful in Ficat and Arlet Stage III hip ON in patients with small- to medium-sized lesions. A review of the results of 30 trapdoor operations performed on 23 patients with Ficat and Arlet Stage III or Stage IV ON of the femoral head performed through a so-called trapdoor made in the femoral head revealed a good or excellent result as determined by the Harris Hip Score system.11
Lightbulb Technique The lightbulb technique uses a cortical window in the anterior aspect of the femoral neck. Necrotic bone can be removed using this window, which can be later packed with nonvascularized bone graft. Wang et al55 evaluated 110 patients (138 hips) who underwent the lightbulb procedure. At mean follow-up of 25 months, mean Harris Hip Scores improved from 62 to 79 points. A total of 94 hips (68%) were considered to have successful outcomes at latest follow-up. Radiographic improvements were noted in 100% of Association Research Circulation Osseous Stage IIa patients, 77% in stage IIb patients, and 51% in stage IIc and IIIa patients.55
Phemister Technique In the Phemister technique, a trephine is inserted through the femoral neck to create a tract to the lesion. A second trephine is then inserted to create another tract to the lesion site. A cortical strut graft can then be placed in the lesion. A recent review reports this procedure to have a clinical success rate ranging from 36% to 90%.25
Total Hip Arthroplasty Once the femoral head has undergone major collapse, replacing the hip joint is the only practical operative option and offers the most predictable pain relief in advanced ON. THA is successful in relieving pain and restoring function in the majority of patients.45–47 In THA, the diseased cartilage and bone constituting the hip joint is replaced with artificial implants made of metal and plastic. A prosthetic hip replacement generally lasts 15 years before it might wear out and need to be revised. For the younger age group, a THA may be a suboptimal solution because of possible activity restrictions. Additionally, because prostheses have longevity restrictions—components wear after long-term use—these patients will likely require a revision THA later in life. THA must be carefully considered and balanced against quality of life issues, but it is not absolutely contraindicated for younger patients.
PATIENT EDUCATION ABOUT HIP OSTEONECROSIS
Prevention of Osteonecrosis
Patient education about risk factors, therapies, and management is essential for patients to make better-informed decisions about their condition. The process of ON education involves identification of an individual’s associated disorders and risk factors related to ON.
Patients with asymptomatic ON may have a high prevalence of progression to symptomatic disease and femoral head collapse. Education for patients with asymptomatic disease is precautionary and imperative to ensure modification of risk factors and optimization of care. Preventing atraumatic ON requires 1) avoiding excessive use of alcohol defined as < 15 drinks/wk for men and < 8 drinks/wk for women,10 2) avoiding smoking, and 3) reducing corticosteroids to the lowest possible therapeutic dose. Informing patients about the correlation between corticosteroid use and potential development of ON is critical in management of this condition.
Prevention of Progression of Osteonecrosis
Patients diagnosed with early-stage ON should be advised of the aforementioned precautions and should avoid placing excessive pressure on their joints, follow a healthy diet, and maintain an appropriate weight to mitigate progression of ON. Although a healthy diet in itself does not directly reduce pressure on a patient’s joints, weight loss (if overweight/obese) will reduce axial loads on the hip joint, which in turn decreases the strain applied to the femoral head/neck (to both the tension and the compression sides).42
CONCLUSION
ON is a pathologic and often painful condition involving necrotic areas of tissue that can affect any bony joint in the body. The hip joint is the most common location for ON and should always be properly evaluated, utilizing radiographic screening and MRI scanning, when ON is initially diagnosed in another body part. The earlier a diagnosis of ON is made, the better the opportunity to save the hip joint without surgical intervention or with minimally invasive surgical techniques.
After a diagnosis of ON is made, the size, extent, and location of the lesion and the classification stages are considered to develop an optimal plan of care. The presence or absence of symptoms is important in this process. The goals of treatment involve attempting to preserve the biological hip joint for as long as possible and consideration of a patient’s lifestyle and quality of life issues. To date, the 2 main therapeutic options for management of hip ON include joint-preserving procedures and THA. Patient education about potential risk factors and development of ON is essential to prevent the condition and/or to potentially prevent or halt progression of early-stage disease to later-stage disease.
本文是陶可版权所有,未经授权请勿转载。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论