
髋关节撞击成像的里斯本Lisbon共识-第一部分:概述(2020)
髋关节撞击成像的里斯本Lisbon共识-第一部分:概述(2020)The Lisbon Agreement on Femoroacetabular Impingement Imaging-part 1: overview
Mascarenhas V V, Castro M O, Rego P A, Sutter R, Sconfienza L M, Kassarjian A, Schmaranzer F, Ayeni O R, Dietrich T J, Robinson P, Weber M A, Beaule P E, Dienst M, Jans L, Lalam R, Karantanas A H, Sudol-Szopinska I, Anderson S, Noebauer-Huhmann I, Vanhoenacker F M, Dantas P, Marin-Pena O, Collado D, Tey-Pons M, Schmaranzer E, Llopis E, Padron M, Kramer J, Zingg P O, De Maeseneer M, Afonso P D. The Lisbon Agreement on Femoroacetabular Impingement Imaging-part 1: overview[J]. Eur Radiol, 2020,30(10): 5281-5297.
转载文章的原链接1:
https://pubmed.ncbi.nlm.nih.gov/32405754/
转载文章的原链接2:
https://link.springer.com/article/10.1007/s00330-020-06822-9
Abstract
Objectives
Imaging assessment for the clinical management of femoroacetabular impingement (FAI) syndrome remains controversial because of a paucity of evidence-based guidance and notable variability in clinical practice, ultimately requiring expert consensus. The purpose of this agreement is to establish expert-based statements on FAI imaging, using formal techniques of consensus building.
由于缺乏循证指导和临床实践中的显著差异,影像学评估对股髋臼撞击(FAI)综合征的临床治疗仍然存在争议,最终需要专家共识。本协议的目的是建立基于专家的FAI成像声明,使用建立共识的正式技术。
Methods
A validated Delphi method and peer-reviewed literature were used to formally derive consensus among 30 panel members (21 musculoskeletal radiologists and 9 orthopaedic surgeons) from 13 countries. Forty-four questions were agreed on, and recent relevant seminal literature was circulated and classified in five major topics (‘General issues’, ‘Parameters and reporting’, ‘Radiographic assessment’, ‘MRI’ and ‘Ultrasound’) in order to produce answering statements. The level of evidence was noted for all statements, and panel members were asked to score their level of agreement with each statement (0 to 10) during iterative rounds. Either ‘consensus’, ‘agreement’ or ‘no agreement’ was achieved.
采用经过验证的德尔菲法和同行评议的文献,从13个国家的30名专家组成员(21名肌肉骨骼放射科医生和9名骨科医生)中正式得出共识。会议就44个问题达成了一致意见,最近的相关开创性文献被分发并分类为五个主要主题(“一般问题”、“参数和报告”、“放射评估”、“MRI”和“超声”),以便产生回答声明。记录了所有陈述的证据水平,并要求小组成员在迭代回合中对每个陈述的同意程度(0到10)进行评分。要么达成“共识”,要么达成“一致”,要么没有达成“一致”。
Results
Forty-seven statements were generated, and group consensus was reached for 45 (95.7%). Seventeen of these statements were selected as most important for dissemination in advance. There was no agreement for the two statements pertaining to ‘Ultrasound’.
共产生了47个陈述,其中45个(95.7%)达成了群体共识。其中17个发言被选为最重要的,以便提前散发。关于“超声波”的两种说法没有达成一致。
Conclusion
Radiographic evaluation is the cornerstone of hip evaluation. An anteroposterior pelvis radiograph and a Dunn 45° view are recommended for the initial assessment of FAI although MRI with a dedicated protocol is the gold standard imaging technique in this setting. The resulting consensus can serve as a tool to reduce variability in clinical practices and guide further research for the clinical management of FAI.
放射学评价是髋关节评价的基础。尽管在这种情况下,专用方案的MRI是金标准成像技术,但推荐骨盆正位X线片和Dunn 45°视图用于FAI的初步评估。由此产生的共识可以作为减少临床实践变异性的工具,并指导FAI临床管理的进一步研究。
Key Points
• FAI imaging literature is extensive although often of low level of evidence.
• Radiographic evaluation with a reproducible technique is the cornerstone of hip imaging assessment.
• MRI with a dedicated protocol is the gold standard imaging technique for FAI assessment.
Introduction
Femoroacetabular impingement (FAI) is a motion-related clinical disorder associated with a triad of insidious onset of groin/hip pain, signs of limited motion and characteristic imaging findings [1, 2] that results from a conflicting contact between the proximal femur and the acetabular rim [1]. This abnormal contact has been associated with hip pain and functional impairment and may ultimately lead to premature osteoarthritis (OA) of the hip [3, 4].
FAI remains controversial in terms of true incidence, diagnosis, prognosis and management [5,6,7]. Despite clinicians becoming increasingly familiar with the concept of FAI, there is no consensus regarding its preoperative diagnostic assessment and FAI case definition. Several groups have put forth important guidelines to better define FAI and related terminology, to facilitate diagnosis and treatment principles [2, 7]. The FAI syndrome (FAIS) concept was introduced in 2016 [7], mainly to emphasize that a clinical triad of symptoms, clinical signs and imaging features must all be present for diagnosis, which is required to ensure that the patient can pursue the optimal treatment strategy [8, 9]. Imaging goals are to diagnose associated soft-tissue damage, to detect early or focally advanced OA and to assess pathologic FAI hip morphologies. The differentiation or quantification of Cam, Pincer and their frequent combination is done on the basis of a predominance of either a femoral or an acetabular abnormality [1, 5, 7, 10].
Previous work reinforced the importance of radiographs on the initial assessment of FAI and advocated the use of cross-sectional imaging to further assess hip morphology as well as cartilage and labral lesions [2, 7, 11]. This has stimulated radiologists as a pivotal part of the diagnostic workup for FAI, leading to an increased use of different imaging techniques (radiographs, computed tomography (CT) and magnetic resonance imaging (MRI)), alone or in combination, alongside with a multitude of imaging signs and parameters [8, 12, 13]. However, to date, imaging assessment for FAI remains non-standardized, because of a paucity of evidence-based guidance, with no consensus among radiology experts and orthopaedic surgeons on which imaging modalities and parameters should be routinely assessed in clinical practice [8, 14]. Consequently, notable variability exists between different practitioners.
The aim of this Delphi-based consensus, ‘The Lisbon Agreement on FAI Imaging’, is to establish expert-based statements on imaging of FAI, using formal techniques of consensus building among an expert group driven by the results of relevant literature review.
这一基于德尔菲的共识,即“FAI成像里斯本共识”的目的,是在相关文献综述的结果驱动下,利用专家小组之间建立共识的正式技术,建立基于专家的FAI成像声明。
Methods
Overview
This consensus is a part of a collaborative project aimed to establish expert-based statements on FAI imaging. Briefly, after project conception (V.V.M., M.O.C. and P.D.A.), the process was started with a first meeting during the European Society of Musculoskeletal Radiology (ESSR) 2018 meeting in Amsterdam, followed by four Delphi rounds, culminating in an open meeting at ESSR 2019 giving rise to ‘The Lisbon Agreement on FAI Imaging’. Panel members gave presentations on the final consensus items at the ESSR 2019 annual meeting (http://www.essr.org) held in Lisbon, Portugal, on June 26–29, 2019. Institutional review board approval was not required for the present consensus as patients were not involved.
Following this first overview, two additional detailed manuscripts will address the totality and specificities of all the statements produced (Part 2—General issues, parameters and reporting; Part 3—Imaging techniques). In this paper, we only report a voted-upon selection of most clinically relevant statements.
The consensus technique
Given the lack of high-level evidence in the literature for FAI imaging assessment, no clinical consensus exists. Accordingly, collecting experts’ opinions in a structured and systematic manner, by using formal consensus development methods such as the Delphi method, is an acceptable way of creating practice recommendations [15, 16]. This method involves a sequence of discussion rounds to determine the opinion of experts on controversial topics, drafted on the basis of the existing literature, to produce a final consensus agreement. Full details of the Delphi method are reported as Supplementary material.
Participants
Both participant groups, orthopaedic surgeons and radiologists, were selected and invited based on specific criteria including (1) previous research in FAI, (2) clinical experience in hip related pathology and FAI and (3) leadership positions in imaging/orthopaedic organizations.
Literature review and question selection
A systematic literature search on relevant databases (PubMed and Cochrane Library) was performed, using the search term ‘femoroacetabular impingement imaging’ from inception to September 2018. Literature was classified in five major groups in order to produce answering statements. The Oxford Centre for Evidence-based Medicine evidence levels were applied [17].
Orthopaedic surgeons were asked to provide relevant clinical FAI imaging–related questions. Each panel member was then asked to include any other question(s) they felt relevant to be included regarding their clinical practice. Forty-four questions were finally agreed on.
Scoring and statistical analysis
Surveys were distributed to participants using the online platform Google Forms® (https://www-google-com-443.vpnm.ccmu.edu.cn/forms/about/). All members were asked to score their level of agreement with each statement (0 to 10).
Minimum statement scoring was considered by the panel if a median ≥ 8 AND interquartile range < 4 were achieved. For these statements, ‘Group consensus’ was further defined as ≥ 80% of voters scoring ≥ 8 and ‘Group agreement’ defined as 67–79% of voters scoring ≥ 8. ‘Lack of agreement’ was assigned if the previous conditions were not met.
Delphi rounds
Statements were scored and commented during iterative rounds while maintaining participant’s anonymity. The consensus process was set to end after 4 rounds or when consensus was met for all statements (whichever occurred first). The aim was to obtain consensus or, if not possible, to measure the degree of agreement for each statement.
Results
A total of 30 panelists were included in this consensus initiative (21 musculoskeletal radiologists and 9 orthopaedic surgeons). Ninety and four tenths (90.4%, 19 out of 21) of radiologists had more than 10 years of experience in the field of musculoskeletal imaging, and 18 of the radiologists had special dedication and/or expertise in hip imaging. All orthopaedic surgeons had more than 10 years of experience in hip preservation surgery (HPS).
Thirty, 28, 27 and 26 participants completed rounds 1, 2, 3 and 4, respectively (6 orthopaedic surgeons and 20 radiologists answered the final round). The overall dropout rate was 13% (33% among orthopaedic surgeons and 5% among radiologists).
A total of 47 statements were generated and distributed among the topics ‘General issues’ (9 items), ‘Parameters and reporting’ (16 items), ‘Radiographic assessment’ (8 items), ‘MRI evaluation’ (12 items) and ‘Ultrasound’ (2 items). At the end of the Delphi process, ‘group consensus’ was obtained for 45 statements. Although level 2 evidence exists regarding the use of ultrasound in the evaluation of FAI, no agreement was reached for the 2 statements on this imaging technique.
In the following paragraphs, we present an overview of ‘The Lisbon Agreement on FAI Imaging’, containing a voted-upon selection of the most clinically relevant topics and statements, followed by a summary of the panel’s discussion (Table 1, Fig. 1).
Table 1 Selection of statements on imaging of femoroacetabular impingement with evidence levels
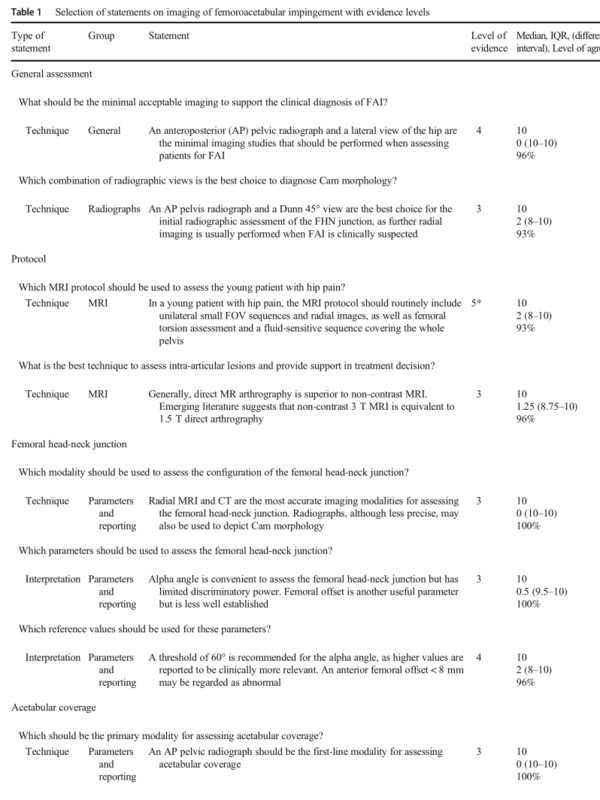
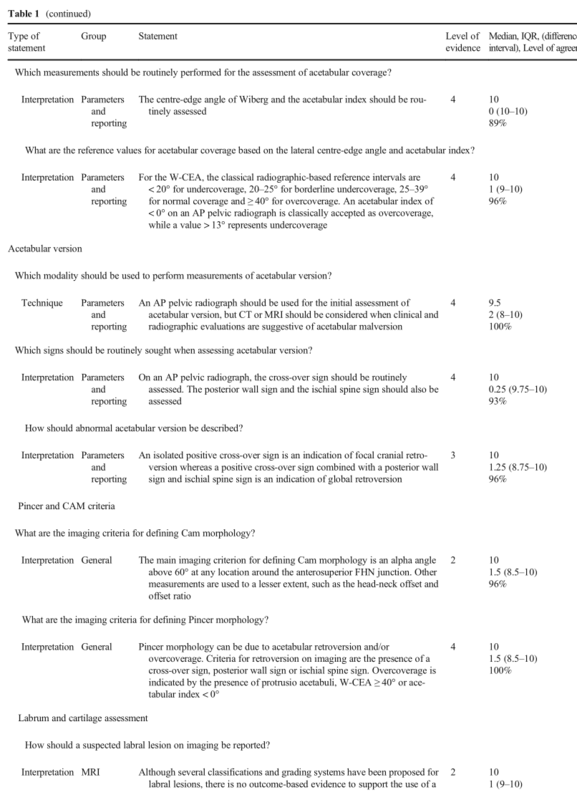
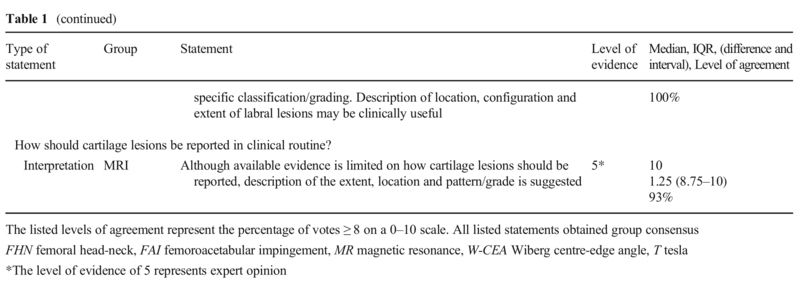
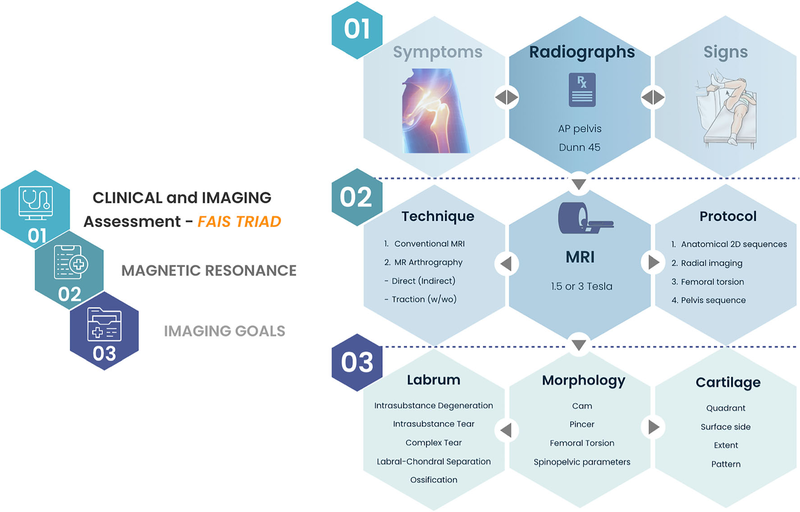
Fig. 1 Pathway for the imaging management and assessment of femoroacetabular impingement syndrome (FAIS). w, with; wo, without; AP, anteroposterior
Discussion
General assessment
Statement:
An anteroposterior (AP) pelvic radiograph and a lateral view of the hip are the minimal imaging studies that should be performed when assessing patients for FAI.
骨盆正位片(AP)和髋关节侧位片是评估FAI患者时应进行的最小影像学检查。
Statement:
An AP pelvis radiograph and a Dunn 45° view are the best choice for the initial radiographic assessment of the femoral head-neck (FHN) junction, as further radial imaging is usually performed when FAI is clinically suspected.
AP骨盆x线片和Dunn 45°视图是对股骨头颈(FHN)连接处进行初步放射学评估的最佳选择,因为当临床上怀疑FAI时通常进行进一步的放射成像。
Radiographs should be used in first-line assessment of patients with suspected FAI, allowing an overall evaluation of the pelvis and hips, as well as exclusion of other causes of symptoms [2, 7]. Conjointly, radiographs and MRI are the standard imaging modalities used to characterize hip pathomorphology and plan treatment [7, 9].
For an initial diagnostic clinical approach, anteroposterior (AP) pelvis and lateral radiographs [2, 7, 8] have been traditionally used and recommended, as the shape and orientation of the acetabulum may be assessed on the AP view and the morphology of the proximal femur best assessed on the orthogonal view of the femoral neck [18] (Fig. 2).
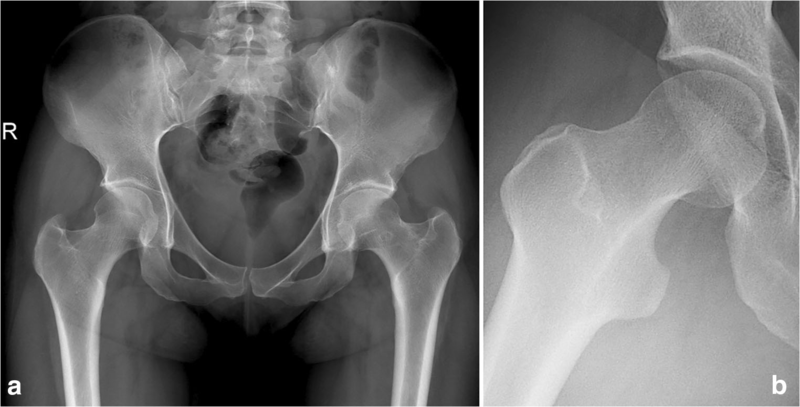
Fig. 2 Minimal recommended radiographic series to evaluate a patient with suspected FAI.
a AP pelvic radiograph. Excessive tilt, obliquity and rotation should be avoided by following a standardized technique. Acetabular coverage and version may be initially assessed in this view.
b Dunn 45° radiograph. It is obtained with the hip in 45° of flexion, 20° of abduction and neutral rotation. This view may be used as first-line assessment of proximal femoral morphologies as it has a substantial correlation with the 1- and 2-o’clock positions defined with cross-sectional imaging
Femoral head-neck (FHN) asphericity in hips with FAI is most often localized in the anterosuperior region [19,20,21]. Although not unanimously accepted, these asphericities are usually best shown with a view with the hips in 45° of flexion and 20° of abduction (Dunn 45° view) [22,23,24,25,26]. The consistent use of this view in the radiographic evaluation of suspected FAIS would provide clinicians with the highest accuracy in demonstrating Cam morphology [22, 25]. However, it is notable that alpha angle (α°) and head-neck offset measurements from these and other radiographic views reportedly reflect only 50% of the overall variation in the shape of the proximal femur [18]. Given that the hip is a 3D anatomic structure, imaging assessment currently used to evaluate pre-arthritic hip conditions is improved by MRI and CT volumetric imaging [27].
FAI髋的股骨头颈(FHN)非球形最常局限于前上区域[19,20,21]。尽管没有被一致接受,但这些非球形性通常在髋关节屈曲45°和外展20°时表现得最好(Dunn 45°视图)[22,23,24,25,26]。在疑似FAIS的影像学评估中一致使用该视图将为临床医生提供显示Cam形态的最高准确性[22,25]。然而,值得注意的是,据报道,这些和其他X线片的α角(α°)和头颈偏移量仅反映了股骨近端形状总体变化的50%[18]。鉴于髋关节是一个三维解剖结构,目前用于评估髋关节关节炎前状况的影像学评估通过MRI和CT体积成像得到改进[27]。
MRI protocol
Statement:
In a young patient with hip pain, the MRI protocol should routinely include unilateral small FOV sequences and radial images, as well as femoral torsion assessment and a fluid-sensitive sequence covering the whole pelvis.
对于髋关节疼痛的年轻患者,MRI方案应常规包括单侧小FOV序列和中心区域的图像,以及股骨扭转评估和覆盖整个骨盆的液体敏感序列。
Statement:
Generally, direct MR arthrography is superior to non-contrast MRI. Emerging literature suggests that non-contrast 3 T MRI is equivalent to 1.5 T direct MR arthrography.
通常,直接MR关节造影优于非对比MRI。新出现的文献表明,非对比的3T MRI相当于1.5 T直接MR关节造影。
There is no definite evidence comparing different imaging protocols or their accuracy [8]. Different authors strive to optimize diagnostic examinations and routinely perform smaller field-of-view (FOV) sequences focusing on a single hip [10, 22, 28] in several imaging planes. Conceptually, acceptable minimum thresholds for adequate spatial resolution are a FOV of 16 cm and a matrix of 256 × 256. If the FOV is larger, matrix must be adjusted accordingly (e.g. for a FOV of 20 cm, the minimum matrix should be 320 × 320).
Panel members agree that radial imaging as well as fast images of the knee and pelvis should be performed to accurately characterize the morphology of the FHN junction and to assess femoral torsion, respectively. A fluid-sensitive sequence with a large FOV covering the whole pelvis should be routinely included, to screen for pathology beyond the hip and overcome potential limitations in clinical assessment, which may result in misguided referrals for hip dedicated imaging. However, whole pelvis imaging must not be regarded as a substitute for focused imaging (e.g. sacroiliac, pubic symphysis) (Fig. 3).
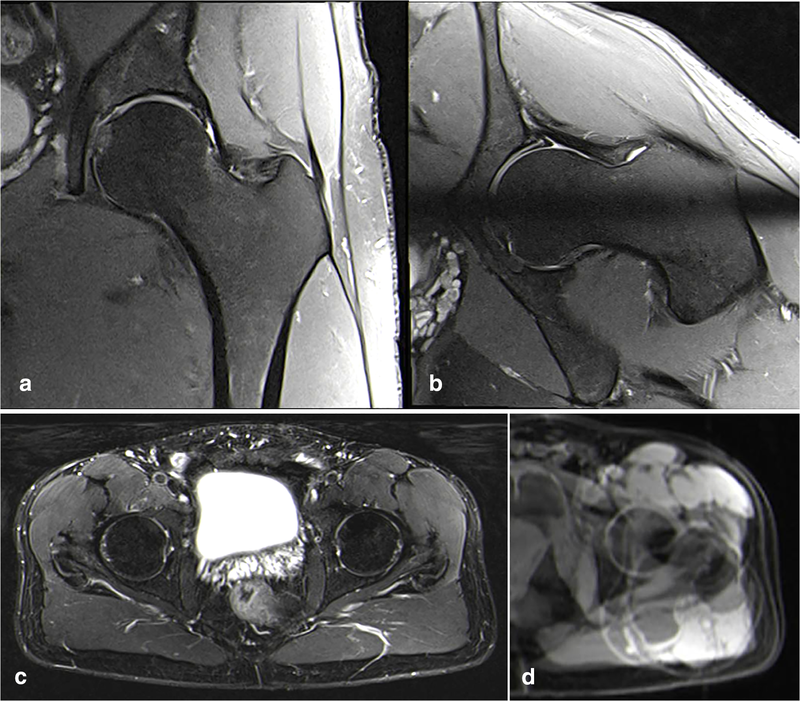
Fig. 3 Sequences that should be included on the proposed routine MRI protocol for the assessment of suspected FAI include unilateral hip 2D sequences (coronal, axial oblique and sagittal are most useful), radial imaging (either a 2D sequence or reformats from a 3D acquisition), a pelvic fluid-sensitive sequence and femoral torsion assessment. Unilateral FOV coronal fat-suppressed proton-density (a) and radial (b) sequences might be used for detailed hip assessment. A 2D large-FOV axial sequence of the pelvis (c) is used to screen for other possible differential diagnoses. Assessment of femoral torsion (d). Different slices may be superimposed on a single image with postprocessing software, making it easy to measure
Radial images rotating around the femoral neck axis allow a circumferential assessment of the hip joint in a clockwise fashion to depict FAI morphologies that are typically located in the anterosuperior quadrant of the FHN junction (3 o’clock to 12 o’clock) [29]. Radial slices can be obtained either through reconstructed 3D volumetric datasets [19, 21] or direct 2D radial sequences based on a sagittal oblique localizer (providing higher-resolution images) [30]. It has been shown that biplanar radiographs do not exclude the presence of a Cam morphology and, additionally, underestimate its severity [11]. Accordingly, the highest correlation between increased α° measured on radial MRI sequences and the Dunn 45° view has been noted [25]. The added value of radial imaging for assessing the acetabulum and/or labrum is not definitely established [31].
Participants in this consensus consider imaging an important factor in treatment decision although its role is mostly limited to characterization of osseous morphology, determination of labral/chondral damage severity and differential diagnoses assessment [1, 7, 32].
For cartilage assessment, radiographs can only indirectly assess chondral pathology by depicting joint space narrowing and secondary OA changes such as subchondral sclerosis/cysts and osteophytes. However, if there are no signs of OA, techniques such as MRI, magnetic resonance arthrography (MRA) and CT arthrography (CTA) appear to help in decision making as they may demonstrate focal/regional cartilage lesions despite minimal radiographic findings. In such cases, these techniques are able to particularly diagnose severe/extensive cartilage damage with acceptable accuracy (those are the lesions that may influence surgical versus non-surgical management) [1, 5, 33].
Unenhanced unilateral hip MRI, direct MR arthrography (dMRA) and less frequently indirect MRA are the techniques of choice for the detection of hip chondro-labral lesions, although the diagnostic test accuracy is superior for dMRA when compared with MRI. Current evidence indicates that dMRA is the best technique to study intra-articular structural lesions [34,35,36] with authors often comparing 1.5 T dMRA to MRI; 3T MRI was reportedly equivalent to 1.5 T dMRA for diagnosing labral tears and cartilage delamination, although superior for diagnosing acetabular cartilage defects [5, 6, 37]. Additionally, 3 T MRI demonstrated similar sensitivity to 3 T dMRA for the detection of acetabular labral tears, although dMRA is more sensitive for detecting acetabular chondral lesions [14, 38]. dMRA can be combined with leg traction to distract the hip joint and has shown encouraging first results [39, 40].
Literature is scarce comparing indirect MRA to MRI, but it shows less overall accuracy of indirect MRA when compared to dMRA [34, 35].
Femoral head-neck junction
Statement:
Radial MRI and CT are the most accurate imaging modalities for assessing the femoral head-neck junction. Radiographs, although less precise, may also be used to depict Cam morphology.
放射MRI和CT是评估股骨头颈交界处最准确的成像方式。射线照相虽然不太精确,但也可用于描绘凸轮形态。
Statement:
Alpha angle is convenient to assess the femoral head-neck junction but has limited discriminatory power. Femoral offset is another useful parameter but is less well established.
α角方便评估股骨头颈交界处,但鉴别力有限。股骨偏移量是另一个有用的参数,但不太确定。
Several reports highlighted the gap in knowledge regarding hip morphology prevalence and its role in the pathogenesis of FAI. FAI-like morphology has been detected in all populations, although few studies use the same case definitions for Cam or Pincer morphology while others used a different definition for males/females [5, 8]. Additionally, other studies use a variety of imaging modalities including radiographs, CT and MRI and measured α° at different FHN positions [1, 5, 7, 10].
Cam morphology corresponds to an asphericity of the FHN junction, most commonly at an anterosuperior location (1–2 o’clock on the clock face), and is usually assessed by measuring the α° [7, 41].
The α° and femoral offset (FO) describe different features of the FHN junction. The α° reflects the proximal aspect of the asphericity, while the FO describes the width of the femoral neck relative to the femoral head [8, 12, 13, 42]. Although these parameters are useful to quantify the FHN junction particularly in a research setting, caution is warranted when using them in routine clinical practice. The use of the α° to quantify Cam morphology is controversial due to its moderate reproducibility, moderate discriminative ability to differentiate patients from healthy subjects and the lack of conclusive data on ideal threshold values [8, 14, 20].
α°和股骨偏移(FO)描述了FHN连接处的不同特征。α°反映了非球形的近端,而FO描述了股骨颈相对于股骨头的宽度[8,12,13,42]。虽然这些参数对量化FHN连接点很有用,特别是在研究环境中,但在常规临床实践中使用它们时需要谨慎。使用α°来量化Cam形态学是有争议的,因为它的可重复性不高,区分患者和健康受试者的能力不高,并且缺乏理想阈值的结论性数据[8,14,20]。
Statement:
A threshold of 60° is recommended for the alpha angle, as higher values are reported to be clinically more relevant. An anterior femoral offset <8 mm may be regarded as abnormal.
α角的阈值建议为60°,因为据报道,较高的阈值与临床更相关。股前偏位< 8mm可视为异常。
Statement:
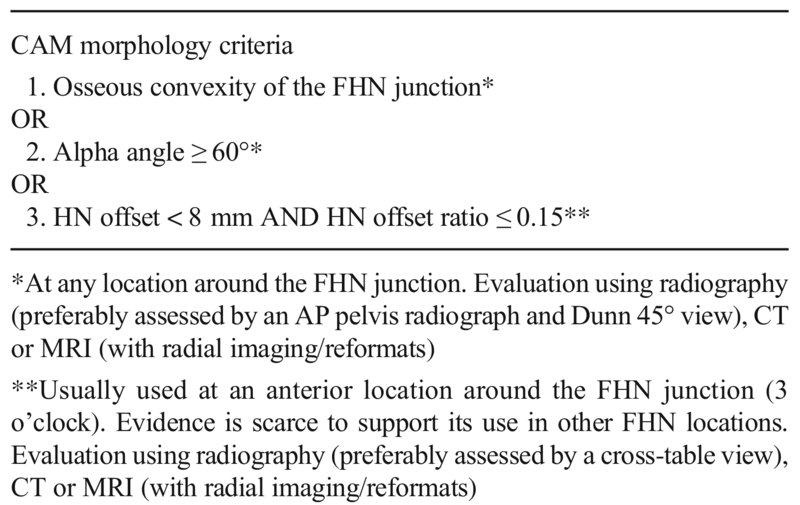
The main imaging criterion for defining Cam morphology is an alpha angle above 60° at any location around the anterosuperior FHN junction. Other measurements are used to a lesser extent, such as the head-neck offset and offset ratio.
确定Cam形态的主要成像标准是在FHN前上连接处周围任何位置的α角大于60°。其他测量的使用程度较低,如头颈偏移和偏移比。
Since the original description of the α° by Nötzli et al, there has been much debate regarding its thresholds [5, 41], although currently, there is evidence that α° thresholds should be defined according to the location around the FHN [5, 19,20,21]. Based on cross-sectional studies comparing asymptomatic volunteers with Cam FAI patients, and on the natural course of FAI (short- and mid-term OA progression in symptomatic hips with α° > 60°), an α° threshold of 60° may be recommended [20, 43]. Recent research suggests that a Cam morphology with α° measurements above 57° to 60° at the 1:30- to 2-o’clock positions is probably symptomatic. Using this threshold would optimize discriminative power while favoring specificity [20, 21]. Conversely, increasing the threshold will increase specificity although decreasing sensitivity.
However, this threshold must be viewed with caution. Several patients with Cam morphology have signs of impingement with α° < 60°, while others above that cut-off will remain asymptomatic [20]. As substantial overlap exists, additional variables should be considered to explain the different clinical manifestations, such as the combination with certain anatomical factors (e.g. decreased femoral antetorsion, acetabular morphology, spinopelvic parameters), sex and athletic performance [19,20,21, 44,44,45,46,48].
Other measurements are used to a lesser extent, such as the FO and offset ratio [13, 22, 49]. There is only very limited data for the FO, but a value of < 8 mm has been reported as abnormal for the anterior FO [13, 9, 50] (Table 2).
Based on these considerations, available evidence and panel consensus, Cam criteria are suggested (Table 2).
Table 2 Criteria proposed by the panel for classifying Cam morphology in a research setting (regardless of the symptomatic state)
Acetabulum assessment
Coverage
Statement:
An AP pelvic radiograph should be the first-line modality for assessing acetabular coverage.
Statement:
The centre-edge angle of Wiberg and the acetabular index should be routinely assessed for the assessment of acetabular coverage.
An AP pelvic radiograph should be the initial examination for assessing acetabular coverage, although cross-sectional imaging may be also used to assess coverage, providing similar measurements for most parameters [51,51,53].
Conflicting reports exist regarding the effect of pelvic positioning on radiographic parameters of coverage [27, 54,54,56], although tilt and rotation seem to mainly influence radiographic signs of acetabular retroversion [57, 58].
The centre-edge angle of Wiberg (W-CEA) and acetabular index (AI) are the most often used parameters of superior-lateral coverage [53, 59]. Anterior and posterior acetabular coverage may be quantified using the anterior and posterior wall indices [60]. Other parameters, such as the anterior centre-edge angle, extrusion index or Sharp angle, are less frequently used [53, 54].
The presence of protrusio acetabuli should always be noted as it is a clinically relevant condition [30, 61]. Coxa profunda, previously regarded as indicative of Pincer morphology, is a common radiographic finding and should be abandoned as a sign of acetabular overcoverage [62].
Statement:
For the centre-edge angle of Wiberg, the classical radiographic-based reference intervals are < 20° for undercoverage, 20–25° for borderline undercoverage, 25–39° for normal coverage and ≥ 40° for overcoverage. An acetabular index of < 0° on an AP pelvic radiograph is classically accepted as overcoverage, while a value > 13° represents undercoverage.
对于Wiberg的中心边缘角,经典的基于X线摄影的参考区间为:欠覆盖< 20°,临界欠覆盖20 - 25°,正常覆盖25-39°,过覆盖≥40°。AP骨盆X线片上髋臼指数< 0°通常被认为是覆盖过广,而> 13°则代表覆盖不足。
The cut-off values for the W-CEA originally reported by Wiberg [63] have been considered gold standard and are recommended by this consensus group.
Wiberg[63]最初报道的W-CEA的临界值被认为是金标准,并被该共识小组推荐。
A recent large population-based study [64] reported reference intervals (RefInt) for the W-CEA of 18–43° for males and 17–42° for females, which are significantly broader compared to the classical W-CEA threshold of < 25° for borderline undercoverage. The same authors reported RefInt for the AI of − 4.7° to 14.8° for males and − 4.1° to 15.6° for females, which are also significantly wider than the classical reference values [65]. Interestingly, if these updated reference values for the AI and for W-CEA were to be used, many hips considered pathologic using the classical RefInt would now be classified as normal. This strongly suggests the need to update the RefInt used in the classification of lateral acetabular coverage based on the natural course of the disease.
最近一项基于人群的大型研究[64]报道了W-CEA的参考区间(RefInt),男性为18-43°,女性为17-42°,与经典的W-CEA阈值< 25°相比,这一阈值明显更宽。同样的作者报告了男性AI的RefInt为- 4.7°至14.8°,女性为- 4.1°至15.6°,这也明显大于经典参考值[65]。有趣的是,如果使用这些更新的AI和W-CEA参考值,许多使用经典的RefInt被认为是病理的髋关节现在将被归类为正常。这强烈提示需要根据疾病的自然病程更新用于髋臼外侧覆盖分类的RefInt。
Other authors defined RefInt in surgically treated symptomatic hips although their application to the asymptomatic general population and its relevance for the natural history of hip disease are yet to be proven (W-CEA/AI: dysplasia < 22°/> 14°, normal coverage 23–33°/3–13°, overcoverage 34–39°/(− 7)–2° and severe overcoverage > 40°/< − 8°) [54].
其他作者将RefInt定义为手术治疗的有症状髋关节,尽管其在无症状一般人群中的应用及其与髋关节疾病自然史的相关性尚未得到证实(W-CEA/AI:发育不良< 22°/> 14°,正常覆盖23-33°/ 3-13°,过度覆盖34-39°/(- 7)-2°,严重过度覆盖> 40°/< - 8°)[54]。
Version
Statement:
An AP pelvic radiograph should be used for the initial assessment of acetabular version, but CT or MRI should be considered when clinical and radiographic evaluations are suggestive of acetabular malversion.
Statement:
On an AP pelvic radiograph, the cross-over sign should be routinely assessed. The posterior wall sign and the ischial spine sign should also be assessed.
Statement:
An isolated positive cross-over sign is an indication of focal cranial retroversion whereas a positive cross-over sign combined with a posterior wall sign and ischial spine sign is an indication of global retroversion.
The most commonly used imaging modality for assessment of acetabular version is the AP pelvic radiograph [53]. Accordingly, surgical planning for correcting abnormal acetabular version has most commonly been based on radiographic signs of retroversion [66,66,68]. Nevertheless, measurements of acetabular version on radiographs were reported to be less reliable (significant number of false positives in assessing retroversion) compared to those obtained in cross-sectional and 3D imaging [69,69,70,72], which may more accurately identify and quantify individual acetabular morphologies. Limitations in conventional radiographic evaluation of acetabular version are both inherent to the imaging technique and related to pelvic tilt [71].
The cross-over sign (COS), posterior wall sign (PWS) and ischial spine sign (ISS) (Fig. 4) should be assessed on radiographs, as there is evidence that depending on the presence of different signs and the degree of acetabular retroversion, different surgical approaches may be considered [73]. In contrast to cranial acetabular retroversion, patients with a global retroversion may benefit from a pelvic reorientation procedure instead of acetabular rim trimming [73]. In fact, there is evidence suggesting that hips with global retroversion (defined as positive COS, PWS and ISS) have a smaller lunate surface and a malrotated acetabulum [74].
交叉征象(COS)、后壁征象(PWS)和坐骨棘征象(ISS)(图4)应在X线片上进行评估,因为有证据表明,根据不同征象的存在和髋臼后翻的程度,可以考虑不同的手术入路[73]。与颅髋臼后倾相反,全髋臼后倾患者可能受益于骨盆重新定位手术,而不是髋臼边缘修整[73]。事实上,有证据表明,髋关节整体后倾(定义为COS、PWS和ISS阳性)的月骨面较小,髋臼旋转不良[74]。
73. Zurmühle CA, Anwander H, Albers CE et al (2016) Periacetabular osteotomy provides higher survivorship than rim trimming for acetabular retroversion. Clin Orthop Relat Res:1–13.
74. Steppacher SD, Lerch TD, Gharanizadeh K et al (2014) Size and shape of the lunate surface in different types of pincer impingement:theoretical implications for surgicaltherapy. Osteoarthritis Cartilage22:951–958.
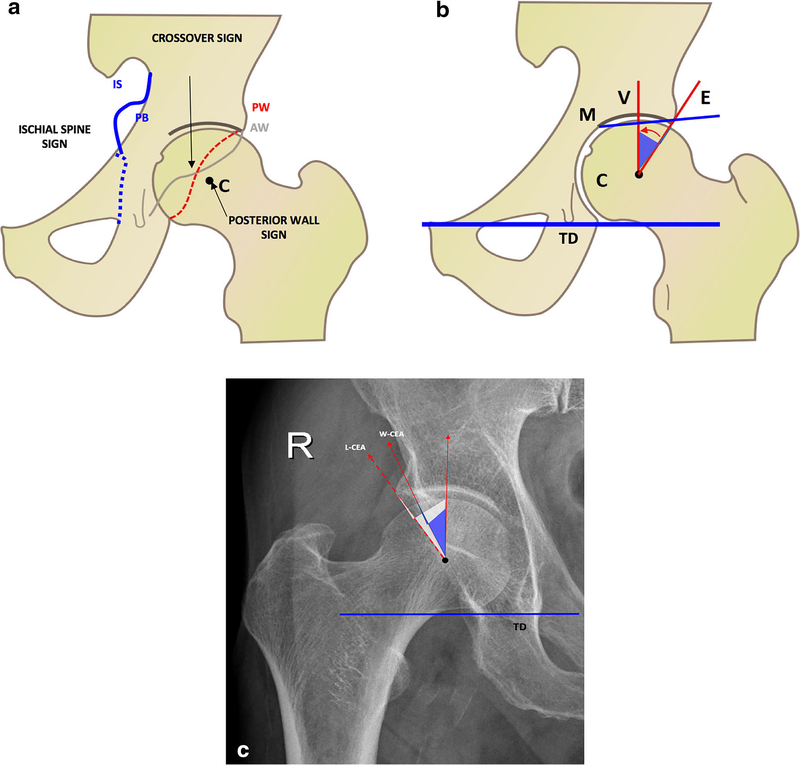
Fig. 4
a The crossover sign is considered positive when the contour of the anterior wall (AW) intersects and becomes lateral to the contour of the posterior wall (PW). The PW sign is considered positive when the projection of the posterior acetabular wall is medial to the projection of the femoral head centre [13]. The ischial spine (IS) sign is considered positive when the projected triangular shape of the IS protrudes, and is visible medially to the pelvic brim (PB).
b Centre-edge angle of Wiberg (W-CEA): an angle formed by a perpendicular line (v) to a line connecting the tear drops (TD), and a line through the centre of the FH (c) and the lateral end of the sourcil (E) (i.e. the sclerotic weight-bearing area of the acetabulum), rather than the lateral rim of the acetabulum. Acetabular index or acetabular inclination: an angle formed by a line connecting the TD, and a line through the medial (M) and lateral edge of the acetabular sourcil (E). c The W-CEA should be distinguished from the lateral centre-edge angle (L-CEA), as the most lateral point to consider would be the lateral end of the sourcil (W-CEA) rather than the most lateral rim of the acetabulum (L-CEA). Frequently, these two reference points might coincide
a当前壁轮廓(AW)相交并成为后壁轮廓(PW)的侧面时,交叉标志被认为是阳性的。当髋臼后壁投影位于股骨头中心投影的内侧时,PW征象被认为是阳性的[13]。当坐骨棘(IS)的三角形突出时,坐骨棘(IS)的征象被认为是阳性的,并且在骨盆边缘(PB)内侧可见。
b Wiberg中心边缘角(W-CEA):由一条垂直线(v)与连接泪滴的直线(TD),以及一条穿过FH中心(c)和源侧端(E)(即髋臼的硬化负重区)的直线形成的角,而不是髋臼的外侧边缘。髋臼指数或髋臼倾斜度:由一条线连接TD和一条线穿过髋臼源体内侧(M)和外侧边缘(E)形成的角度。
c W-CEA应与外侧中心边缘角(L-CEA)区分开来,因为需要考虑的最外侧点是源体的外侧端(W-CEA)而不是髋臼最外侧边缘(L-CEA)。这两个参考点经常会重合
Caution is warranted, however, as (a) these radiographic signs are commonly present among asymptomatic subjects [62, 75, 76], (b) their accuracy per se is questionable [69, 71] and (c) radiographs may overestimate acetabular retroversion. Advanced imaging should thus be considered when clinical findings and radiographs are consistent with Pincer FAI and retroversion, although its clinical added value remains to be established.
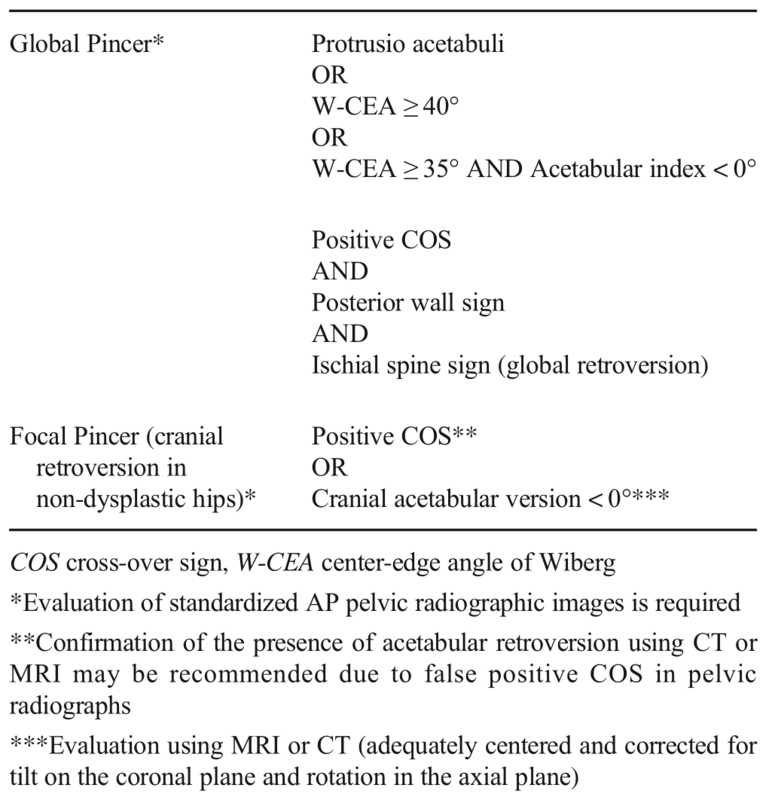
PINCER criteria
Statement:
Pincer morphology can be due to acetabular retroversion and/or overcoverage. Criteria for retroversion on imaging are the presence of a cross-over sign, posterior wall sign or ischial spine sign. Overcoverage is indicated by the presence of protrusio acetabuli, W-CEA ≥ 40° or acetabular index < 0°.
钳形形态可能是由于髋臼后移和/或过度覆盖。影像学检查的标准是出现交叉征、后壁征或坐骨棘征。如果存在髋臼前突,W-CEA≥40°或髋臼指数< 0°,则表明覆盖过广。
Imaging signs of Pincer morphology include markers of increased acetabular coverage and of abnormal acetabular version. Caution is warranted when interpreting radiographs, as pelvic tilt and rotation are known to affect some of these parameters, particularly AP coverage and retroversion [57]. Although generally supported by the literature [53], high-quality research is needed in order to more precisely define the value of radiographic signs in the diagnosis of Pincer morphologies (particularly the COS, PWS and ISS), as well as the clinical relevance of cross-sectional imaging in this setting. Based on the above-mentioned rationale, published evidence and panel consensus, Pincer criteria are suggested (Table 3).
Table 3 Criteria proposed by the panel for classifying Pincer morphology in a research setting (regardless of the symptomatic state)
Labrum and cartilage assessment
Labrum
Statement:
Although several classifications and grading systems have been proposed for labral lesions, there is no outcome-based evidence to support the use of a specific classification/grading. Description of location, configuration and extent of labral lesions may be clinically useful.
虽然已经提出了几种针对唇部病变的分类和分级系统,但没有基于结果的证据支持使用特定的分类/分级。描述唇部病变的位置、形态和范围可能在临床上有用。
Several surgical and MRI-based classifications for the description of labrum lesions have been proposed [77,77,79]. Currently, no evidence supports the use of a specific description of labral injury based on treatment outcomes. Due to the weak agreement between these classifications, imaging assessment of the acetabular labrum may instead focus on an accurate descriptive report, including location, configuration and extent of labral tears and associated cartilage and osseous changes [39] (Table 4, Fig. 5).
Table 4 Recommended descriptors of labral injury, based on inferential evidence [34, 38, 40]
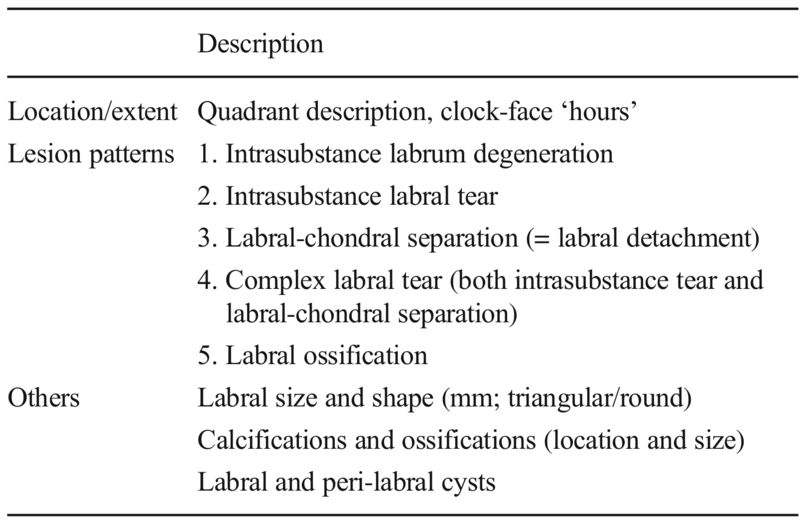
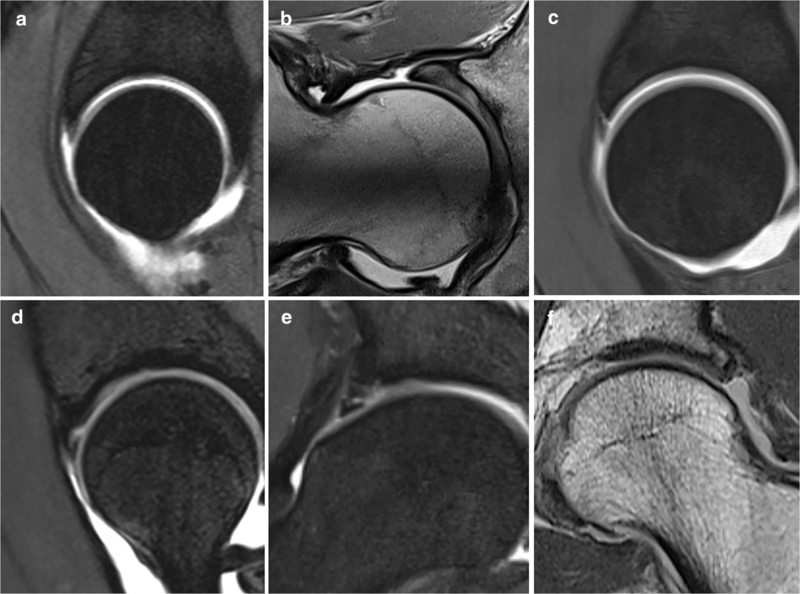
Fig. 5 Labrum tear patterns.
a Intrasubstance labrum degeneration, sagittal plane.
b Intrasubstance labrum degeneration and hypertrophy, radial plane at 1.5 o’clock.
c Labral-chondral separation (= labral detachment), sagittal plane.
d Intrasubstance labrum tear, sagittal plane.
e Complex labral tear (both intrasubstance tear and labral-chondral separation), coronal plane.
f Labral ossification, coronal plane
Cartilage
Statement:
Although available evidence is limited on how cartilage lesions should be reported, description of the extent, location and pattern/grade is suggested.
Currently, there is only outcome-based evidence supporting the description of the extent of cartilage damage, while only inferential evidence is available for the remaining features. Nevertheless, description of the location, surface and pattern/grade is recommended by the panel of experts (Table 5, Fig. 6).
Table 5 Recommended descriptors of cartilage lesions on a hip MRI study
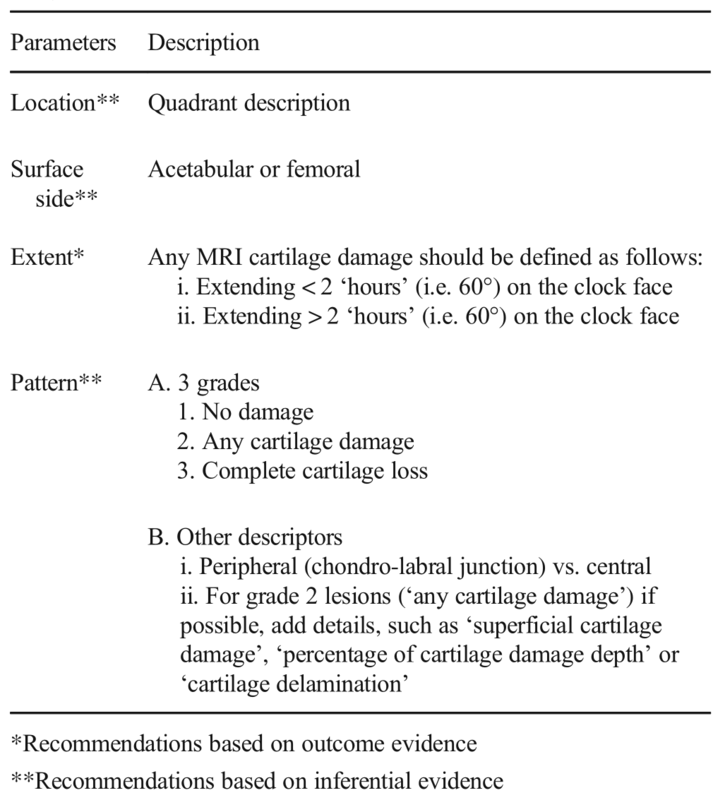
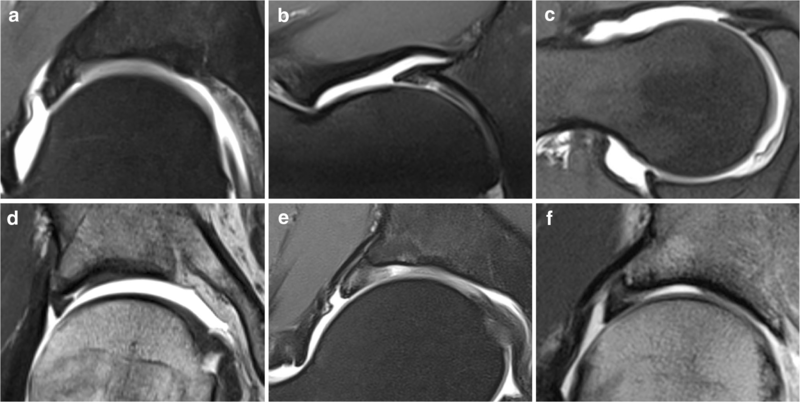
Fig. 6 Cartilage lesion patterns.
a Grade 1, ‘no damage’ (normal thickness cartilage).
b Grade 2, ‘any cartilage damage’ (acetabular focal partial thickness cartilage defect).
c Grade 2, ‘any cartilage damage’ (femoral head superficial cartilage damage).
d Grade 2, ‘any cartilage damage’ (peripheral acetabular chondral delamination involving the chondro-labral junction).
e Grade 3, ‘complete cartilage loss’ (focal full-thickness acetabular cartilage defect).
f Grade 3, ‘complete cartilage loss’ (diffuse full-thickness acetabular cartilage loss)
The extent of cartilage damage evaluated by MRA is reportedly an independent prognostic factor for long-term outcome of FAI surgery (worse if greater than 60° around the clock face) [61]. In the presence of extensive cartilage loss, some surgeons may choose not to perform corrective FAI surgery.
The pattern of cartilage lesion can also affect surgical planning including the technique and timing of cartilage repair (e.g. abrasion/microfracture versus autologous cartilage transplantation) and potential concomitant intra-articular and additional extra-articular procedures.
Location has also diagnostic and surgical planning implications. Femoral cartilage damage (a) is a poor prognostic factor, (b) is indicative for progressive joint degeneration and (c) is easier to treat with open surgery than with hip arthroscopy [80, 81]. In addition, the (a) typically located lesions support a Cam or Pincer FAI mechanism and corresponding treatment, and (b) posterior lesions are difficult to access arthroscopically [82]. Conversely, atypically located lesions may support other etiologies (e.g. trauma, overuse) [10].
Conclusion
In conclusion, the first international, multidisciplinary Delphi-based consensus for imaging of FAI was developed. We critically reviewed the available evidence, the roles and limitations of each technique, highlighted recommended protocols, imaging parameters, classifications and criteria. The resulting consensus statements can serve as a tool to reduce variability in preoperative, intraoperative and postoperative practices and guide further research for the clinical management of FAI.
总之,第一个国际性的、多学科的基于delphi的FAI成像共识已经形成。我们严格审查了现有的证据,每种技术的作用和局限性,强调了推荐的方案,成像参数,分类和标准。由此产生的共识声明可以作为减少术前、术中和术后实践差异的工具,并指导FAI临床管理的进一步研究。
Abbreviations
2D:Two-dimensional
3D:Three-dimensional
α°:Alpha angle
AI:Acetabular index
AP:Anteroposterior
COS:Cross-over sign
CT:Computed tomography
CTA:CT arthrography
dMRA:Direct MR arthrography
ESSR:European Society of Musculoskeletal Radiology
FAI:Femoroacetabular impingement
FAIS:Femoroacetabular impingement syndrome
FHN:Femoral head-neck
FO:Femoral offset
FOV:Field-of-view
HPS:Hip preservation surgery
ISS:Ischial spine sign
MRA:Magnetic resonance arthrography
MRI:Magnetic resonance imaging
OA:Osteoarthritis
PWS:Posterior wall sign
RefInt:Reference intervals
W-CEA:Centre-edge angle of Wiberg

本文为转载文章,如有侵权请联系作者删除。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论