论文精选
发表者:李黎波 人已读
Lasers Med Sci (2009) 24:981–984
DOI 10.1007/s10103-009-0653-8
Treatment of perianal Paget’s disease using photodynamic therapy with assistance of fluorescence examination:
case report
Lasers Med Sci (2009) 24:981–984
DOI 10.1007/s10103-009-0653-8
L. Li (*) : L. Zhang :W. Liao : R. Luo
Department of Oncology, Nanfang Hospital,
Southern Medical University,
Guangzhou 510515, People’s Republic of China
e-mail: li_libo2008@yahoo.com.cn
Y. Deng
Department of Pathology, Nanfang Hospital,
Southern Medical University,
Guangzhou, People’s Republic of China
Z. Huang
Department of Radiation Oncology,
University of Colorado Denver,
Aurora, CO, USA
Abstract Our aim was to determine the usefulness of
fluorescence examination and photodynamic therapy (PDT)
for the management of perianal extramammary Paget’s
disease. A 75-year-old woman underwent two courses of
PDT. The first treatment was carried out with topically
applied 5-aminolevulinic acid (ALA) to the affected area
(2.5×2.5 cm2) 3 h before light treatment. We used ALA/
protoporphyrin IX (PpIX)-mediated fluorescence to visualize
the lesion and its margins. The lesion was treated with a
630 nm laser at 120 J/cm2. Forty days later, the residual
lesion was given a second treatment at the same light dose
after topical application of ALA and intravenous injection
of HiPorfin. ALA/PpIX-mediated fluorescence served as a
useful tool to visualize the lesion’s location. Complete cure
was achieved after the second course of PDT. During
7 months of follow up, no recurrence, scarring or functional
loss was noticed. We concluded that ALA-assisted fluorescence
examination can be a useful tool to determine the
lesion and its margins. ALA-PDT is effective for superficial
lesions, but, for thicker and deeper lesions, the systemic
administration of photosensitizer is needed.
Keywords Perianal extramammary Paget’s disease .
Photodynamic therapy. Fluorescence examination
Introduction
The incidence of perianal extramammary Paget’s disease is
rare and often misdiagnosed as eczema or dermatitidis. In
some patients it remains as a local disease for several years
without spread and metastasis. It has usually been present
for a long time before biopsy is performed to confirm its
diagnosis. Because of the low morbidity, no treatment
guideline based on evidence-based medicine or multicenter
study can be followed. Surgical excision is the main choice
for non-invasive perianal Paget’s disease [1]. However,
many patients have a long history and a large lesion, which
might have invaded the anus, scrotum or vulva simultaneously.
Their treatment involves extensive resection and
skin transplantation. For patients who need an artificial anus,
their life quality can be severely affected by surgical trauma
and slow recovery. Furthermore, the high relapse rate after
surgery is also problematic. Other modalities, such as
radiotherapy, carbon dioxide (CO2) laser thermal ablation,
and local or systemic chemotherapy, are often unsatisfactory
[2–4]. Therefore, there is an urgent need for us to find
an effective modality to treat perianal Paget’s disease.
Photodynamic therapy (PDT) is a relatively new therapy,
which involves the light activation of a photosensitizer
inside a tumor. Photons are absorbed by the photosensitizer,
which triggers the photosensitizer to enter into an excited
state. The excited photosensitizer can then pass its energy
to oxygen molecules to generate singlet oxygen (1O2),
which attacks cellular components and structures through
oxidation and subsequently causes cell death [5]. The
selective accumulation of photosensitizer in tumor cells and
the local irradiation of the lesion site might make PDT an
ideal non-invasive focal therapy for extramammary Paget’s
disease. The feasibility of PDT for the treatment of
extramammary Paget’s disease has been studied in a small
number of patients since the mid-1990s [6]. Various PDT
protocols have also been used in China [7, 8]. Recently, we
successfully treated one case of perianal Paget’s disease
with two-courses of PDT with the assistance of a
fluorescence diagnosis. Here, we report our experience of
this case.
Case report
A 75-year-old female Chinese patient with complaints of
perianal erythema, papular eruption, effusion and pruritus
was initially admitted to the Dermatology Department of
our hospital. She had received surgical treatment for her
hemorrhoid 1 year previously. Physical examination
showed that there were sporadic edema erythema, papular
eruption, and dissipated and mild effusion over an area of
2.5×2.5 cm2 in the perianal region (Fig. 1a). Histopathological
examination of serial biopsies confirmed the
characteristic changes of perianal Paget’s disease: diffused
or patch epithelial infiltrate consisting of pleomorphic cells
with abundant pale-staining cytoplasm and large transparent
nuclei. In addition, laboratory examinations showed
tumor cells that were positive for alcian blue–periodic acid
Schiff (AB-PAS) staining, cytokeratin (CK), CK8 and
human melanoma black (HMB45) and negative for CK7
and S-100, respectively. A computed tomography (CT) scan of
the abdomen and pelvic areas and a whole-body bone emission
computed tomography (ECT) were carried out to exclude
tumor metastasis. The patient declined surgery and was
transferred to the Oncology Department for PDT treatment
with the hope of saving the structure and function of the anus.
We prepared a fresh solution of aminolevulinic acid
(ALA) solution (20%) by dissolving ALA powder (Shanghai
Fudan-zhangjiang Bio-Pharmaceutical Co., Ltd.) in
physiological saline solution. The lesion plus a 2 cm
margin were covered by ALA-soaked gauzes for 3 h.
Before PDT light irradiation, lesion locations were visualized
by fluorescence examination using a light emitting
diode (LED) (MC-405PDD-HL-1, Shenzhen Sanqiu Technology
Ltd.) emitting ultraviolet (UV) light at 405 nm.
ALA’s fluorescent product, protoporphyrin IX (PpIX),
showed a characteristic bright brick-red color (Fig. 1b).
Images were taken by a digital camera equipped with a
green filter. The fluorescence-positive region plus a 1 cm
margin was light irradiated with a diode laser (630 PDT
laser, Diomed) and through a microlens fiber (Diomed) at a
dose level of 120 J/cm2.
The PDT was repeated on the second day, since there
were still tumor lesion residuals at the edges of the primary
lesion and near the anus that were visible under fluorescence
examination after topical application of ALA for 3 h.
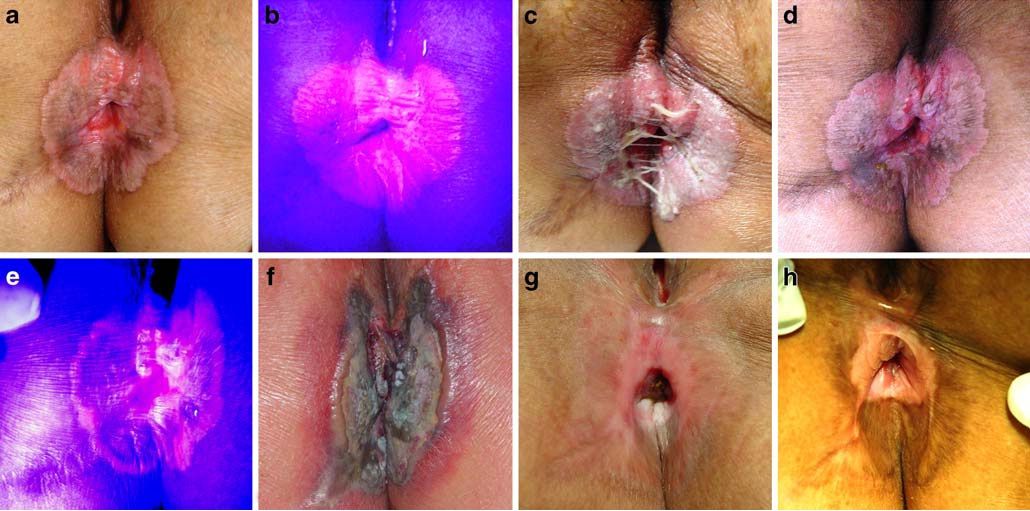
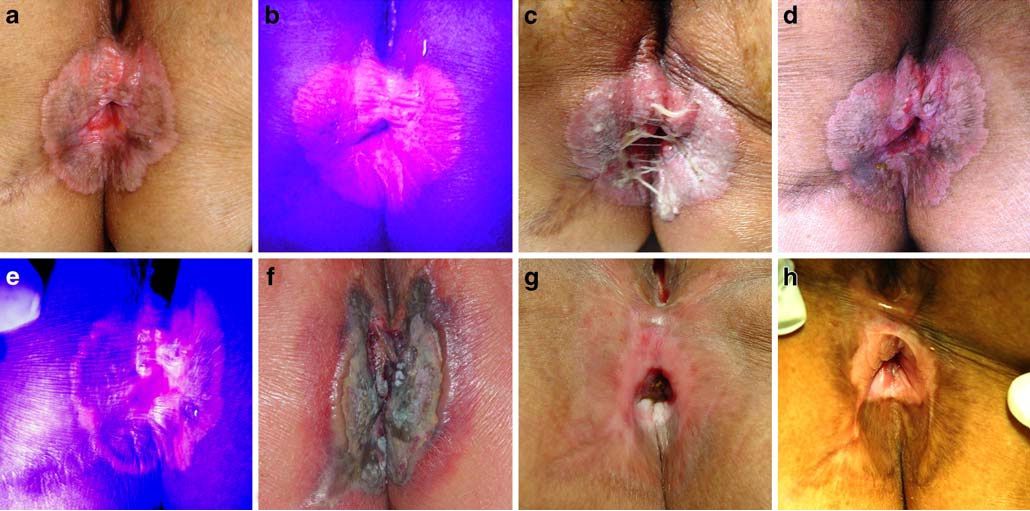
Fig. 1 Visual and fluorescence examinations before and after
treatment. a, b Visual and fluorescence view of the lesion before the
first session of PDT. c One week after ALA-PDT. d, e Visual and
fluorescence view of lesion before the second session of PDT. f One
week after the second session of PDT. g Three months after PDT.
h Seven months after PDT
982 Lasers Med Sci (2009) 24:981–984
Light irradiation was repeated for the residual lesions at the
same dosage of 120 J/cm2. Tumor necrosis was observed
1 week after the ALA-PDT (Fig. 1c).
Examination 40 days after the ALA-PDT showed that
there were still erythema annulare in the perianal area, with
a clear edge. The lesion scale was similar to that prior to
ALA-PDT (Fig. 1d). Therefore, we decided to use a more
rigorous PDT protocol by combining topical application of
ALA and intravenous administration of HiPorfin (Chongqing
Huading Modern Bio-Pharmaceutical Co., Ltd.).
HiPorfin is a Chinese version of hematoporphyrin derivatives
(HpD) [9]. It was given intravenously at a dose of
5 mg/kg 48 h before light irradiation. ALA solution was
applied topically to the lesion 3 h before light irradiation, as
described before. Fluorescence examination showed that
there was still fairly strong red fluorescence at the edge of
the primary lesion and near the anus (Fig. 1e). Light
irradiation of 120 J/cm2 was carried out as described before.
The tumor lesion had deeper necrosis 7 days after the
second session of PDT (Fig. 1f).
The examination 3 months after the second session
showed that the tumor lesion had disappeared completely
and the skin had healed well (Fig. 1g). Follow-up
examination 7 months after the PDT showed that the
treatment area was free of visible lesion or scar (Fig. 1h).
Biopsy confirmed that there was no tumor presence in the
treated area. The patient was satisfied with the treatment,
which had preserved the anus and its function.
Discussion
Compared with conventional surgery, chemotherapy and
radiotherapy, PDT has many advantages, such as being
non-invasive or minimally invasive, having low toxicity,
better cancer selectivity, and the ability to be repeated. We
have successfully treated various cancers using Photofrin
and other PDT photosensitizers. PDT can cure early stage
cancer and prolong the survival of patients suffering late
stage cancer [10].
ALA is a precursor to heme in the heme cycle. When
excess ALA is supplied to tissues, malignant tumor cells
can take up the exogenous ALA and convert it to a
fluorescent photosensitizer, protoporphyrin IX (PpIX).
Monitoring the distribution of PpIX is a useful tool for
visualizing tumor locations, since the ALA-induced PpIX
fluorescence accumulates primarily in malignant tumor
tissue and its fluorescence is much stronger than that in
the normal skin [11]. ALA/PpIX is regarded as a great
breakthrough for cancer diagnosis and treatment [12]. It can
be a useful tool to determine size and margin in perianal
Paget’s disease [13, 14]. Furthermore, several previous
reports have also demonstrated that the topical application
of ALA-PDT is an effective option for superficial lesions
and mucosal surfaces [6, 8, 15]. Topical ALA application is
advantageous because it does not cause dermal damage and
long-lasting skin photosensitization. Healing times associated
with ALA-PDT are short. However, for bulky disease,
thicker and deeper lesions, and disease on the axilla, groin,
vulva or scrotum, intralesional injection of ALA or
intravenous administration of photosensitizer (e.g. Photofrin)
might be considered [6, 7, 16].
Because of the nature of this case, surgery would have
cut off the normal skin 3 cm beyond the tumor lesion,
which would have been followed by skin transplantation
and installation of an artificial anus [17, 18]. As an
alternative, the patient chose PDT, in order to avoid surgery.
Initially, we thought the lesion was superficial, so we used
topical application of ALA only. Fluorescence examination
showed that the tumor lesion was more extensive. ALAPDT-
induced necrosis was shallow—possibly due to the
limited tissue penetration of ALA, although ALA-PDT is
effective in eliminating superficial lesions [8]. The patient’s
skin had healed fairly quickly, 1 month after PDT, but there
were still residual tumors (see Fig. 1d).
For the second course of PDT, we used two photosensitizers
(i.e., the topical application of ALA and the
systematic application of HiPorfin) in order to identify
residual lesion and ablate thicker and deeper lesions. This
regimen indeed produced deeper necrosis (see Fig. 1f);
therefore, the skin healing time was longer. Complete
healing took nearly 3 months. Since the perianal lesion was
close to the anus, bowl movement and feces might also
have affected healing. Nonetheless, the combination modality
eliminated the lesion completely, and there was no
recurrence during a 7-month follow-up. More importantly,
PDT preserved the anus and its function.
Although limited case reports and pilot studies suggest
that the topical application of ALA solution or emulsion
formulations are effective, well tolerated, and easy to apply
for the examination and treatment of superficial lesions,
ALA bioadhesive patches and ALA ester derivatives (e.g.,
methyl ester) have been used for vulval Paget’s disease and
have produced reliable outcomes [19, 20]. Nonetheless,
based on the therapeutic advantages of PDT demonstrated
by others and this study, the topical and/or systemic
application of PDT should be considered an effective offlabel
alternative treatment for the management of Paget’s
disease at various locations and of various severities.
In summary, ALA/PpIX-assisted fluorescence examination
can be a useful tool to determine the lesion’s margin
and residual tumors and to ensure that the PDT treatment
covers the entire tumor lesion. ALA-PDT is a simple and
effective approach for superficial lesions, but for thicker
and deeper lesions, systemic administration of photosensitizer
is needed. Furthermore, PDT shows the advantage of
Lasers Med Sci (2009) 24:981–984 983
preserving the anus and its function in treating perianal
Paget’s disease.
本文是李黎波版权所有,未经授权请勿转载。 本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅
发表于:2011-08-02