图文文章
发表者:陶拓宇 人已读
肌电图
肌电图是神经系统检查的延伸,它是通过电刺激神经、针扎入肌肉来检查神经、肌肉是否有问题一门技术。一般包括神经传导和针级肌电图。肌电图是一种主观性极强客观检测手段。不同检查者有可能得出完全不同的结论。
肌电图分狭义和广义肌电图。狭义肌电图是指用同芯圆针刺入肌肉,观察肌肉电位变化又叫针极肌电图。广义肌电图包括针极肌电图、神经传导、重复神经电刺激(repetitive nerve stimulation,RNS)、F波、H反射、瞬目反射(blinkreflex)、单纤维肌电图
(single fiber electromyograhy,SFEMG)、运动单位计数、巨肌电图和诱发电位。通常所说肌电图指的是广义肌电图。神经肌肉电生理与广义肌电图范畴相同。
肌电图检查的适应证
1.前角细胞及其以下(包括前角细胞、神经根、神经丛、周围神经、神经肌肉接头和肌肉)病变的诊断和鉴别诊断。
2.肌肉内注射肉毒毒素部位的选择(部分患者)。
3.需要与中枢神经疾病鉴别。
肌电图检查的安全性和注意事项
1.必须使用二相电源插座和插头供电,并保证插座的地线完整 。
2.遵守仪器使用的安全要求,由专业人员定时检查设备的漏电情况,当出现触摸设备外壳有电击样感觉或电源线破损等情况时,应及时停止操作。
3.不要将刺激电极置于心脏区域,刺激电极、记录电极和地线应置于肢体同一侧,以减少通过躯体的泄露电流。
4.对于意识障碍或存在感觉障碍的患者,要特别注意,避免意外损伤。
5.在进行肌电图检查时,不要再将其他与电源线连接的设备与患者相连或接触,除非经过专业人员检查确保安全。测定过程中不应让患者接触肌电图一设备外壳或面板。
6.对于存在出血倾向的患者,应仔细评估肌电图检查的利弊。如果血小板低于50000/mm3,或抗凝治疗时凝血酶原国际标准化比值为 1.5一2.0,采用针电极检查时,出血的风险增加,如果决定检查,建议先检查位置表浅的小肌肉,观察出血情况。血友病或其他遗传性凝血功能障碍疾病患者应避免进行肌电图检查,除非己经提前纠正凝血功能异常。
7.对于安装有心脏起搏器的患者,不应进行 NCS。
8.体内植人了心律转复设备或除颤器时,应咨询心脏专科医生,刺激器要远离植人设备15cm以上,必须接好地线,并且刺激电流的时限不应超过0.2ms。
9.肋间神经或Erb点针电极刺激、颈棘旁肌、隔肌、前锯肌等肌电图检查时,要注意判断检查的利弊,慎重选择,严格规范操作,避免气胸。
10.对于疑诊Creutzfeldt一Jakob病的患者,应使用一次性电极,检查结束后所有与血液接触过的物品均要妥善处理。
11.对于HIV和乙型肝炎病毒感染患者,进行针电极检查时,建议使用一次性电极,对于非一次性电极要按照要求进行消毒处理。检查人员在检查时以及处理电极时要注意自身防护。
肌电图价值
1.肌电图能解决神经系统受损定位定性问题如腰疼定位急性腰疼怎么治?,也能对神经损伤恢复进行预测如经典型GBS即脱髓鞘型预后好影响格林巴利(GBS)预后的因素(修订3),轴突型预后差;面神经轴突损害预后差原发性面瘫面瘫(Bell面瘫)预后;神经外伤出现再生电位预示神经再生等。
2.肌电图能对某些神经肌肉病起到确诊的作用如运动神经元病无感觉障碍但运动功能受损需要考虑以下几种疾病、重症肌无力重症肌无力激素怎么用?,GBS等。
3.与中枢神经疾病鉴别,没有神经肌肉病就意味是中枢神经疾病,如脊髓型颈椎病、中风、心理等。
4.可以鉴别肌萎缩是费用性还是病理性肌无力或/和肌萎缩怎么办?。
对肌电图检查者的基本要求
1.检查者应熟悉神经解剖知识。
2.检测前应进行详细的神经系统检查,确立检查方案。
3.检查前向患者解释:(1)检测过程中保持肢体放松状态,尽量避免精神紧张;(2)检测过程中随着电刺激量的增加会有不适的感觉,运动NCS 测定时会有肌肉收缩的动作;(3)针电极检查会有疼痛等。
4.肌电图检查之前应常规进行NCS。
肌电图检查方案
肌电图是临床检查的延续,不同疾病肌电图检查方案不同。卡压神经病如腕管,一般查双侧上肢神经正中、尺、桡神经传导就可以了,但有时需要查针级肌电图排除神经根等其它疾病。运动神经元病除了四肢神经传导外,还需要查四肢、头面颈部针级肌电图。重症肌无力除了神经传导外,还需要查重复电刺激、单纤维肌电图。
没有临床知识很难判断是什么疾病,因而也很难确定肌电图检查方案,没有临床诊断,做肌电图就犹如没有指南针在大海上航行。另外肌电图特点就是主观性极强,特别是关于纤颤和正锐波识别,没有大量实践是很难做到的,这也是肌电图结果不同的人检查差异很大主要原因。因此,一个合格肌电图医生必须熟知常见神经肌肉病、神经肌肉解剖和亲自做过肌电图检查而且诊断过。
运动神经传导
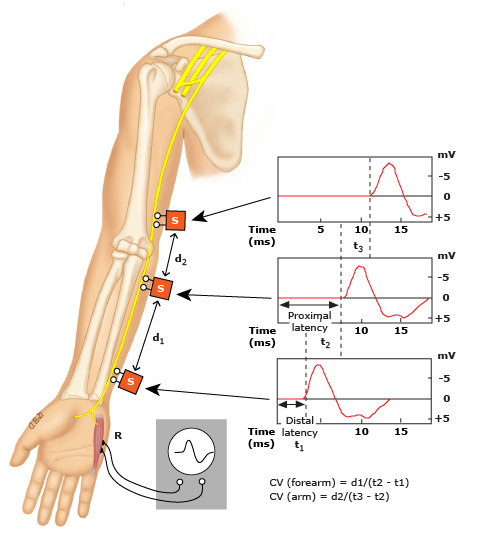
Stimulation at different proximal sites along the ulnar nerve while recording from the abductor digiti minimi muscle allows the conduction velocity (CV) of the motor neurons to be calculated.
感觉神经传导
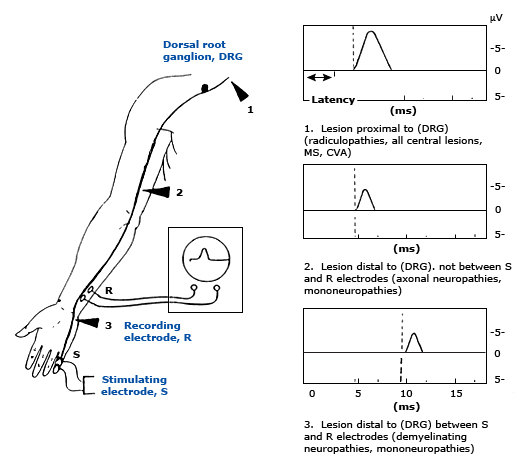
Recording of the sensory action potential is helpful in determining the site of nerve injury particularly in those with lesions resulting in sensory symptoms. This illustration depicts a sensory nerve conduction study of the ulnar nerve. Normal latency is seen with lesions of the central nervous system or those that are proximal to the dorsal root ganglion (arrowhead number 1). A more distal lesion (arrowhead number 2) results in a decreased amplitude but normal conduction velocity. Either a compressive mononeuropathy (arrowhead number 3) or generalized demyelinating peripheral neuropathy results in a decrease in both amplitude and conduction velocity.
神经传导异常形式-波形弥散
With increasing lengths of nerve segment between stimulating and recording electrodes, temporal dispersion increases and amplitude decreases.
A: Stimulus onset.
B: CMAP onset.
C: Peak amplitude of negative phase.
D: Return to baseline.
E: Peak of positive phase.
F: Return to baseline.
A-B: Latency.
B-C: Rise time.
B-C-D: Area under the curve.
B-D: Duration of negative phase.
C-E: Peak-to-peak amplitude.
运动单位
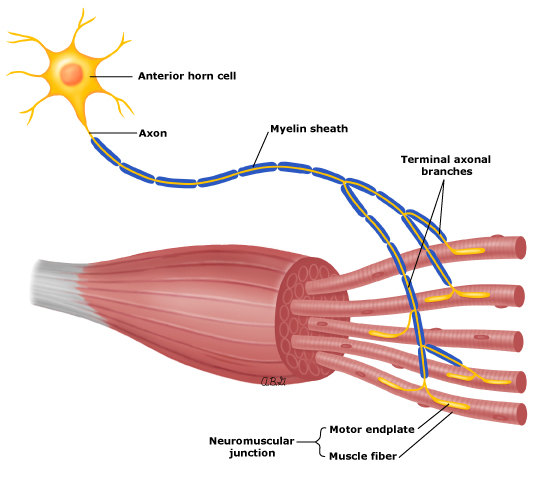
不同位置运动单位不同
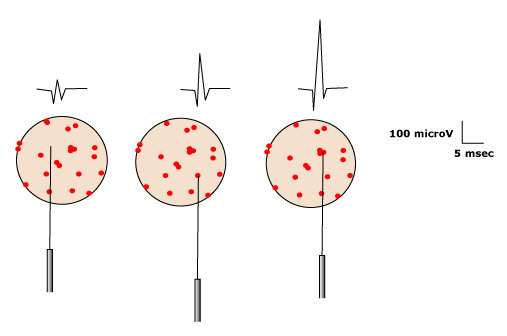
Of all MUAP parameters, amplitude is most dependent on needle position. Only muscle fibers very close to the needle contribute to amplitude, as opposed to duration, wherein most muscle fibers contribute. Note change in amplitude as needle is moved to different locations within the same motor unit.
Reproduced with permission from: Preston, DC, Shapiro, BE. Electromyography and neuromuscular disorders, Butterworth-Heinemann, Boston 1998. Copyright © 1998 Elsevier.
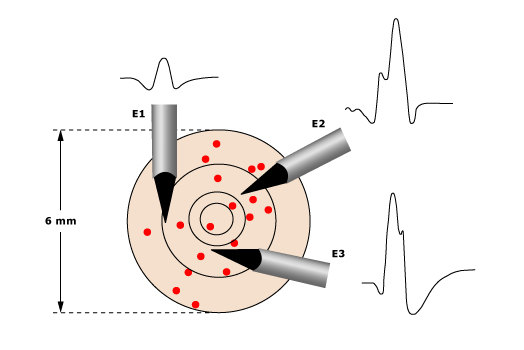
The position of the EMG needle influences the morphology of the recorded MUAP. To properly assess MUAP parameters, the major spike must be as steep as possible, indicating the proximity of the needle to the motor unit. Note that needle electrode position E3 has the shortest major spike rise time and is the preferable position in which to assess the MUAP. Also note that although MUAP amplitude changes markedly with needle position (compare position E1 with E3), duration is relatively unaffected. (From D Dimitru, JA DeLisa. AAEM minimonograph #10: volume conduction. Muscle Nerve 1991;14:605. Reprinted by permission of Wiley.)
Reproduced with permission from: Preston, DC, Shapiro, BE. Electromyography and neuromuscular disorders, Butterworth-Heinemann, Boston 1998. Copyright © 1998 Elsevier.
运动单位测量
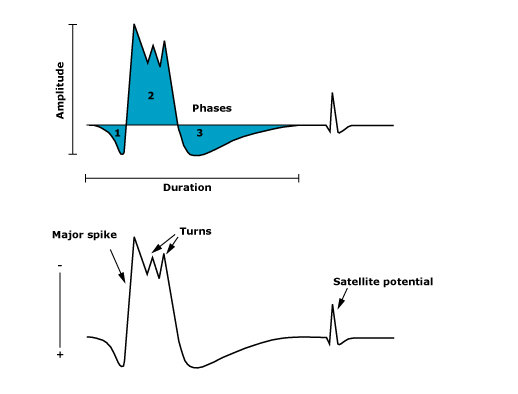
Duration is measured as the time from the initial deflection of the MUAP from baseline to its final return to baseline. It is the parameter that best reflects the number of muscle fibers in the motor unit. Amplitude reflects only muscle fibers very close to the needle and is measured peak to peak. Phases (shaded areas) can be determined by counting the number of baseline crossings and adding 1. MUAPs are generally triphasic. Serrations (also called turns) are changes in direction of the potential that do not cross the baseline. The major spike is the largest positive-to-negative deflection, usually occurring after the first positive peak. Satellite, or linked, potentials occur after the main potential and usually represent early reinnervation of muscle fibers.
Reproduced with permission from: Preston, DC, Shapiro, BE. Electromyography and neuromuscular disorders, Butterworth-Heinemann, Boston 1998. Copyright © 1998 Elsevier.
异常针级肌电图-正锐波和纤颤电位
In (A) and (B) the sweep is free running. The traces in (B) represent a continuation of the EMG signal after the last trace in (A). In (C), the waveforms from (A) and (B) are superimposed using amplitude trigger and delay line. Calibration is 200 microV/division and 10 ms/division in (A) and (B), and 100 microV/division and 1 ms/division in (C).
Reproduced with permission from: Nandedkar SD, Barkhaus PE, Sanders DB, Stalberg EV. Some observations on fibrillations and positive sharp waves. Muscle Nerve 2004; 23:888. Copyright ©2004 John Wiley & Sons Inc.
正常、神经源损害、肌源性损害肌电图特点
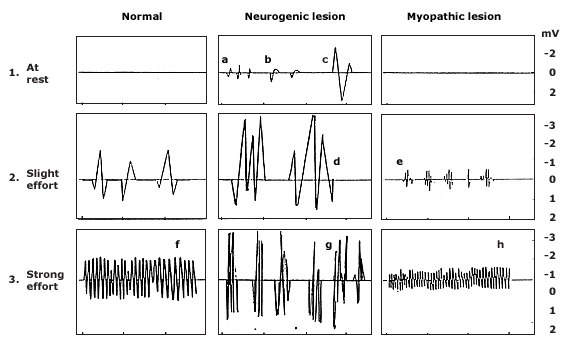
1. At rest (spontaneous activity): a. fibrillations, b. positive sharp waves, c. fasciculation.
2. Slight effort (motor unit potentials): d. giant polyphasic, e. BSAPS (brief-small-abundant polyphasic).
3. Strong effort (interference pattern): f. full, g. reduced units, h. reduced amplitude.
* helpful in selecting denervated muscles in radiculopathies (myotomal), mononeuropathies (distal to lesion), generalized neuropathies (distal muscles), and myopathies
我们是怎么做好肌电图?
1.肌电图与临床关系密切和主观性强,决定我们以下检查过程。
2.坚持谁做谁发报告,因为在肌电图检查过程中很多信息判断是很主观的,有些是不能在报告中反映出来的,我见过很多肌电图报告有很多名人签名,其中不乏有顶尖三甲医院,但经过时间的检验其结论是错的,因为原始资料有误;
3.对于每一个病人,要询问病史和体检,形成初步临床诊断;
4.根据初步诊断确定肌电图检查方案,在检查过程有时因检查与临床诊断不符,考虑新的诊断重新修正检查方案;
5.对所做的资料,在报告中提及是否有神经肌肉损害,先提出肌电图诊断再结合临床提出疾病诊断或诊断方向;
6.向病人解释结果,为病人下一步诊治提供参考依据,交代复查时间,做好追踪工作。
本文是陶拓宇版权所有,未经授权请勿转载。 本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅
发表于:2012-04-23