 三甲
三甲
年轻股骨颈骨折患者术后股骨头坏死:16%发生股骨头坏死,发生时间为术后1~7年,平均3.8年
年轻股骨颈骨折患者术后股骨头坏死:16%发生股骨头坏死,发生时间为术后1~7年,平均3.8年:2020年J Orthop Surg Res
一项对250名患者平均随访7.5年的回顾性研究
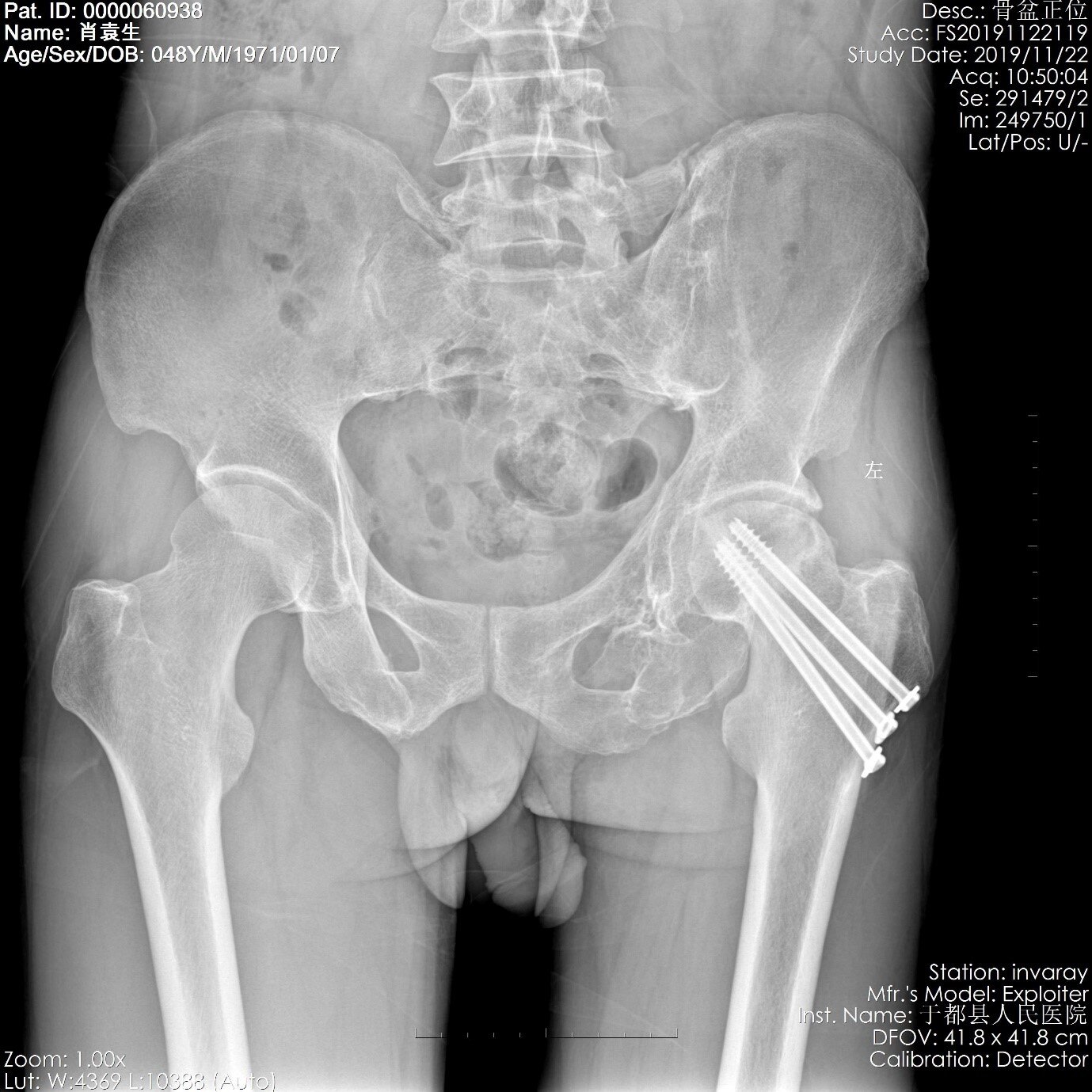
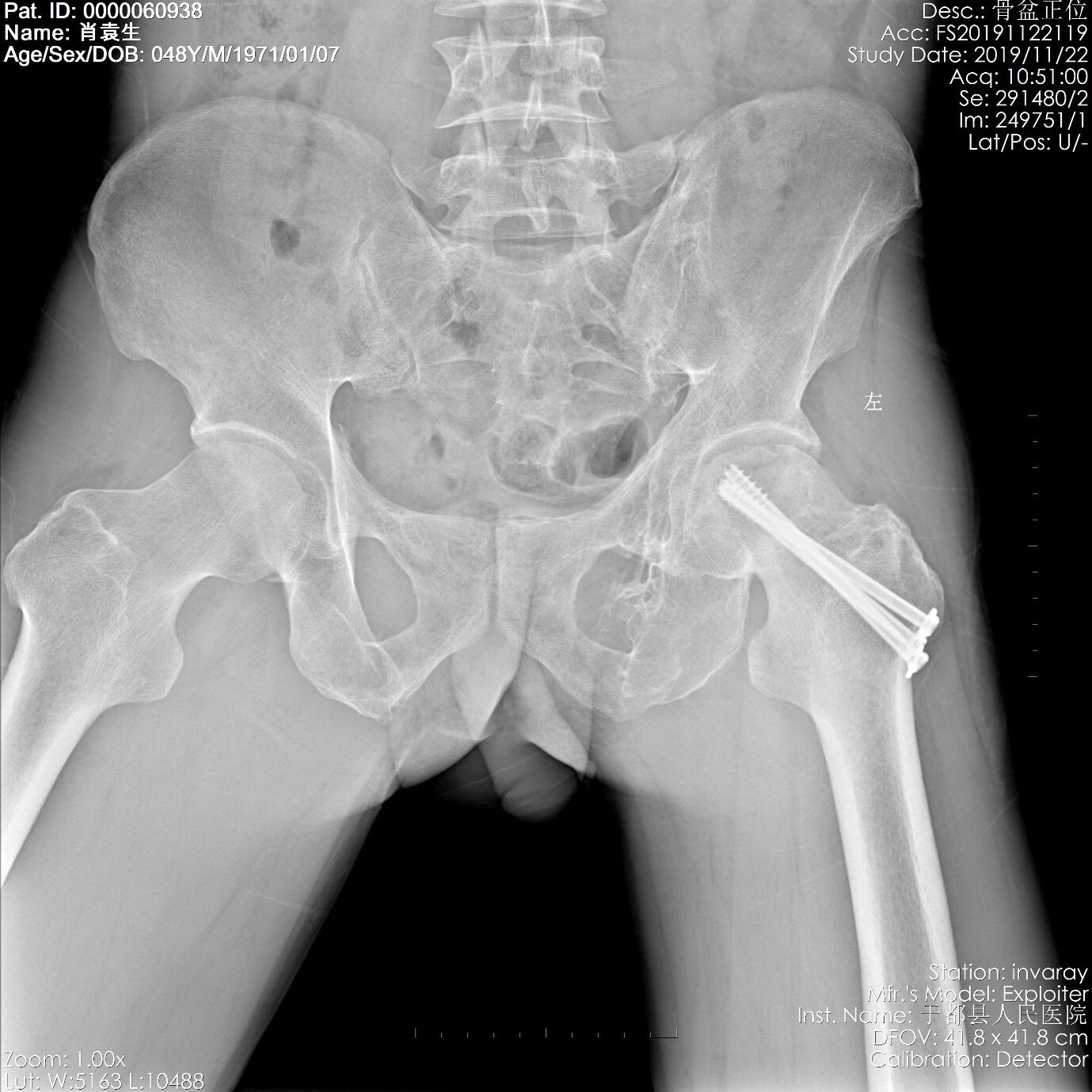
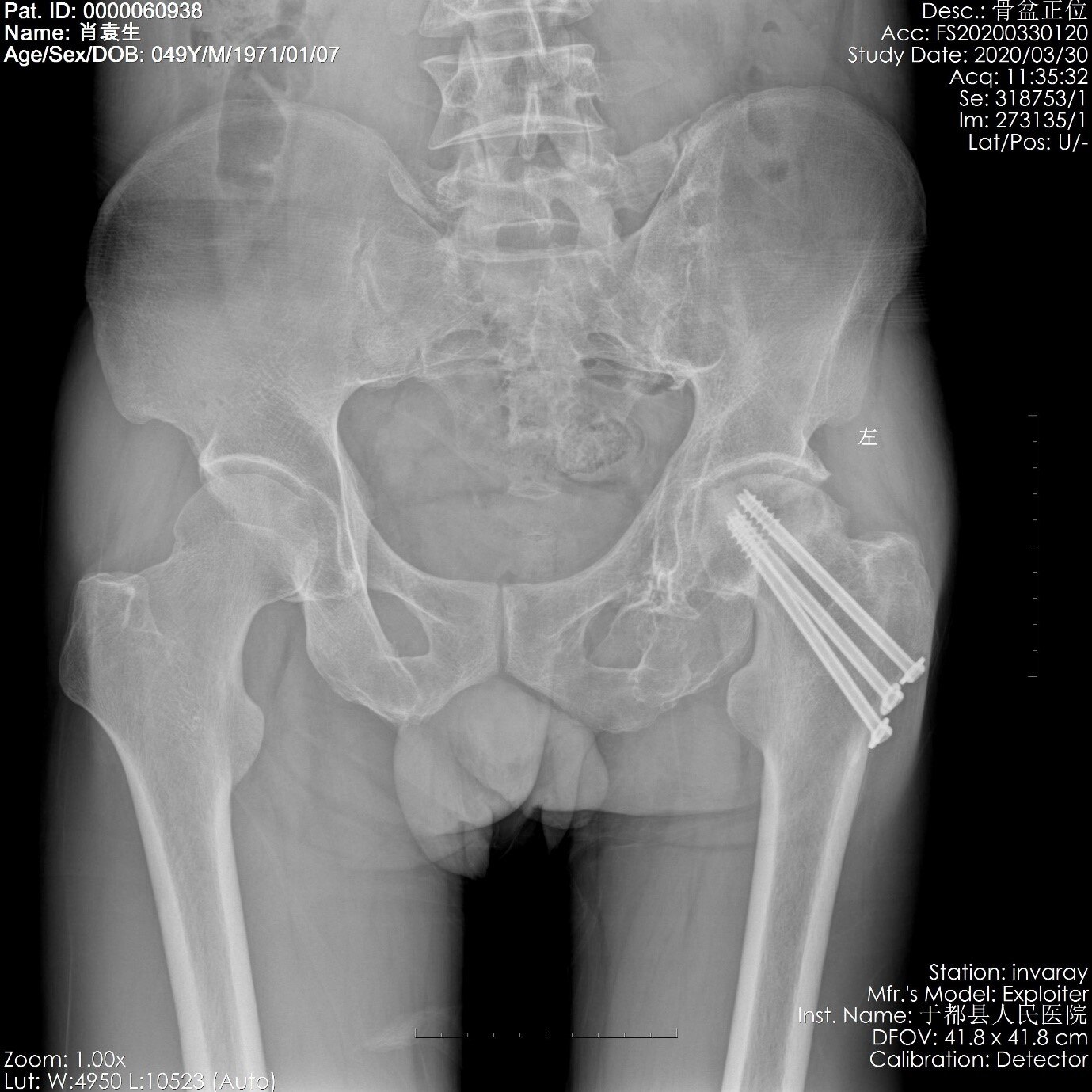

图A-D典型股骨颈骨折术后股骨头坏死病例:中年男性,47岁,因2018年4月外伤致左髋部疼痛伴活动受限,双侧髋关节正侧位X线片示左侧股骨颈骨折(Garden IV型),入院后给予完善相关检查,予以闭合复位空心拉力螺钉内固定术,术后未能定期复诊。后于2019年11月22日因患侧髋部行走后站立疼痛,至门诊复诊拍片,显示已发生股骨头坏死(ARCO IIIA期-2019版指南)。于2020年04月07日因左股骨颈骨折术后2年要求取内固定经门诊收入院。入院查体:身高165公分,体重:59千克;跛行步态。左髋部可见陈旧性手术疤痕,无红肿,局部无压痛,左髋及左膝关节活动正常,皮下未及内固定物,左下肢远端血运运动感觉未及异常。2020-03-30我院X线提示:左股骨颈骨折骨性愈合,左股骨头无菌性坏死,左髋关节骨关节炎。2020年04月09日取出内固定后复查拍片,可见股骨头负重区明显坏死(ARCO IIIA期-2019版指南)股骨头颈结合区有骨赘增生,但关节间隙未见明显狭窄,髋臼侧未见骨赘增生硬化改变。
(主诊医师:黄小华副主任医师,赣州市于都县人民医院)
作者:Fang Pei, Rui Zhao, Fenglei Li, Xiangyang Chen, KaiJin Guo, Liang Zhu.
作者单位: Department of Orthopaedic Surgery, Mayo Clinic, Rochester, Minnesota.
译者:陶可(北京大学人民医院骨关节科)
摘要
目的:探讨60岁以下患者股骨颈骨折手术治疗后股骨头坏死(ONFH)的危险因素。
方法:对2002年1月至2016年1月在徐州市3家医院收治的250例股骨颈骨折病例进行研究。随访1~15年,回顾性分析股骨颈术后股骨头坏死的临床资料。记录危险因素,包括年龄、性别、术前牵引力、受伤至手术时间、复位方法、复位类型、BMI、ASA分类和复位质量。采用Logistic回归分析评估股骨颈骨折治疗后发生ONFH的独立危险因素。
结果:随访时间1~15年,平均7.5年。250例患者中没有骨折不愈合,但40例(16%)股骨头坏死。股骨头坏死时间为术后1~7年,平均3.8年。单因素分析显示,骨折类型、复位质量、拆除内固定物、BMI和ASA分级是影响股骨颈骨折患者股骨头坏死的危险因素,差异有统计学意义(P < 0.05)。多因素分析显示,内固定治疗、骨折类型(移位)、复位质量(不满意)、BMI(>25)、ASA分级(III+IV)是影响股骨颈骨折患者股骨头坏死的独立危险因素。
结论:成人股骨颈骨折空心加压螺钉术后存在多种股骨头坏死的高危因素。内固定物的拆除、骨折类型、复位质量、BMI和ASA分级是影响股骨头坏死发生的最重要的危险因素。在治疗过程中,应有一些针对性的措施,降低股骨头坏死的发生率。
关键词:股骨颈骨折;内固定;股骨头坏死;风险因素。
文献出处:Fang Pei, Rui Zhao, Fenglei Li, Xiangyang Chen, KaiJin Guo, Liang Zhu. Osteonecrosis of femoral head in young patients with femoral neck fracture: a retrospective study of 250 patients followed for average of 7.5 years. J Orthop Surg Res. 2020 Jun 29;15(1):238. doi: 10.1186/s13018-020-01724-4.
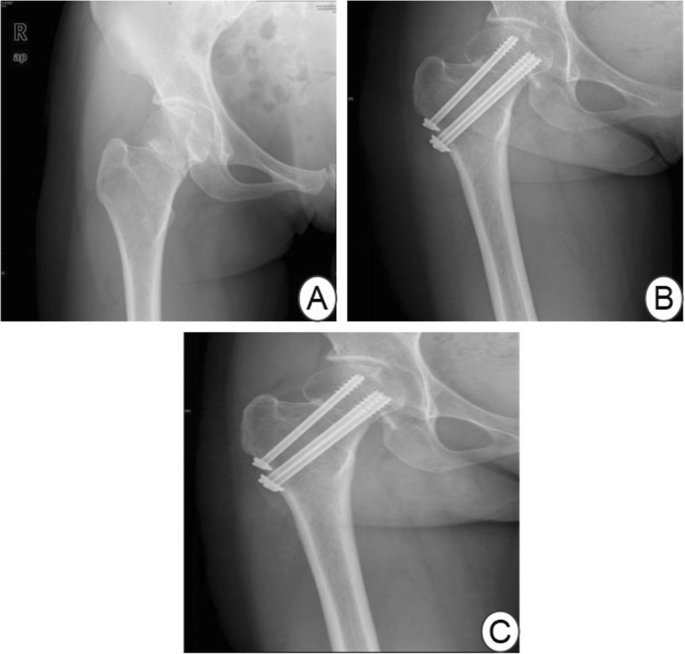
Figure 1 a Preoperative X-ray film. b At 1 year after the operation, X-ray examination showed that the necrosis of the right femoral head. c At 2 years after the operation
图1 a术前X线片。b术后1年 线检查示右侧股骨头坏死。c术后2年
Osteonecrosis of femoral head in young patients with femoral neck fracture: a retrospective study of 250 patients followed for average of 7.5 years.
Abstract
Objective: To investigate the risk factors for osteonecrosis of the femoral head (ONFH) after the treatment of femoral neck fracture in patients under 60 years old.
Methods: A total of 250 cases of femoral neck fracture treated at 3 hospitals in Xuzhou from January 2002 to January 2016 were studied. The patients were followed up for 1~15 years, and the clinical data on femoral head necrosis after the femoral neck operation were analysed retrospectively. Risk factors were recorded, including age, gender, preoperative traction, time from injury to operation, reduction method, type of reduction, BMI, ASA classification, and quality of reduction. Logistic regression analysis was used to evaluate the independent risk factors for ONFH after treatment of femoral neck fracture.
Results: The duration of follow-up was 1~15 years, with an average of 7.5 years. None of the 250 patients had fracture non-union, but 40 (16%) had necrosis of the femoral head. The time to necrosis of the femoral head was 1~7 years after the operation, with an average of 3.8 years. Univariate analysis showed that the type of fracture, the quality of reduction, the removal of internal fixation, BMI and ASA classification were risk factors affecting necrosis of the femoral head in patients with femoral neck fracture, and the difference was statistically significant (P < 0.05). Multivariate analysis showed that internal fixation, fracture type (displacement), reduction quality (dissatisfaction), BMI (> 25), and ASA grade (III + IV) were independent risk factors affecting femoral head necrosis in patients with femoral neck fracture.
Conclusion: A variety of high-risk factors for femoral head necrosis are present after surgery with hollow compression screws for femoral neck fracture in adults. Removal of internal fixation, type of fracture, quality of reduction, BMI, and ASA classification were the most important risk factors influencing the development of femoral head necrosis. During treatment, there should be some targeted measures to reduce the incidence of necrosis of the femoral head.
Keywords: Femoral neck fracture; Internal fixation; Osteonecrosis of the femoral head; Risk factors.
本文是陶可版权所有,未经授权请勿转载。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论