 三甲
三甲
髌腱病(髌腱炎,跳高者膝,蹲走者膝)的康复锻炼方案:2020年J Musculoskelet Neu
髌腱病(髌腱炎,跳高者膝,蹲走者膝)的康复锻炼方案:2020年J Musculoskelet Neuronal Interact杂志
作者:Qassim I Muaidi.
作者单位: Department of Physical Therapy, College of Applied Medical Sciences, Imam Abdulrahman Bin Faisal University, Dammam, K.SA.
译者:陶可(北京大学人民医院骨关节科)
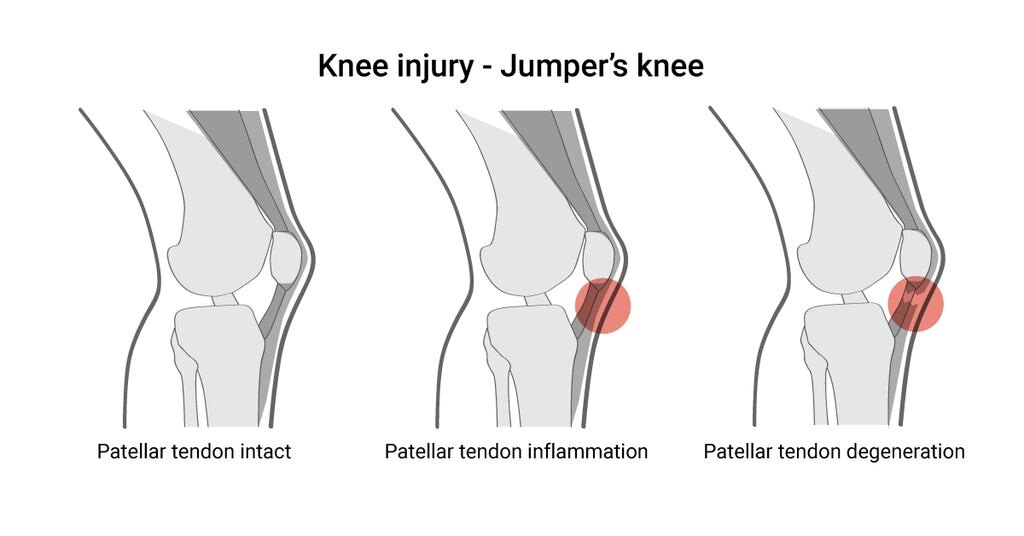
髌腱病(髌腱炎,跳高者膝,蹲走者膝)主要分为三个不同的病理阶段:髌腱完整性良好,髌腱炎性病变,髌腱退性改变,甚至发生断裂。
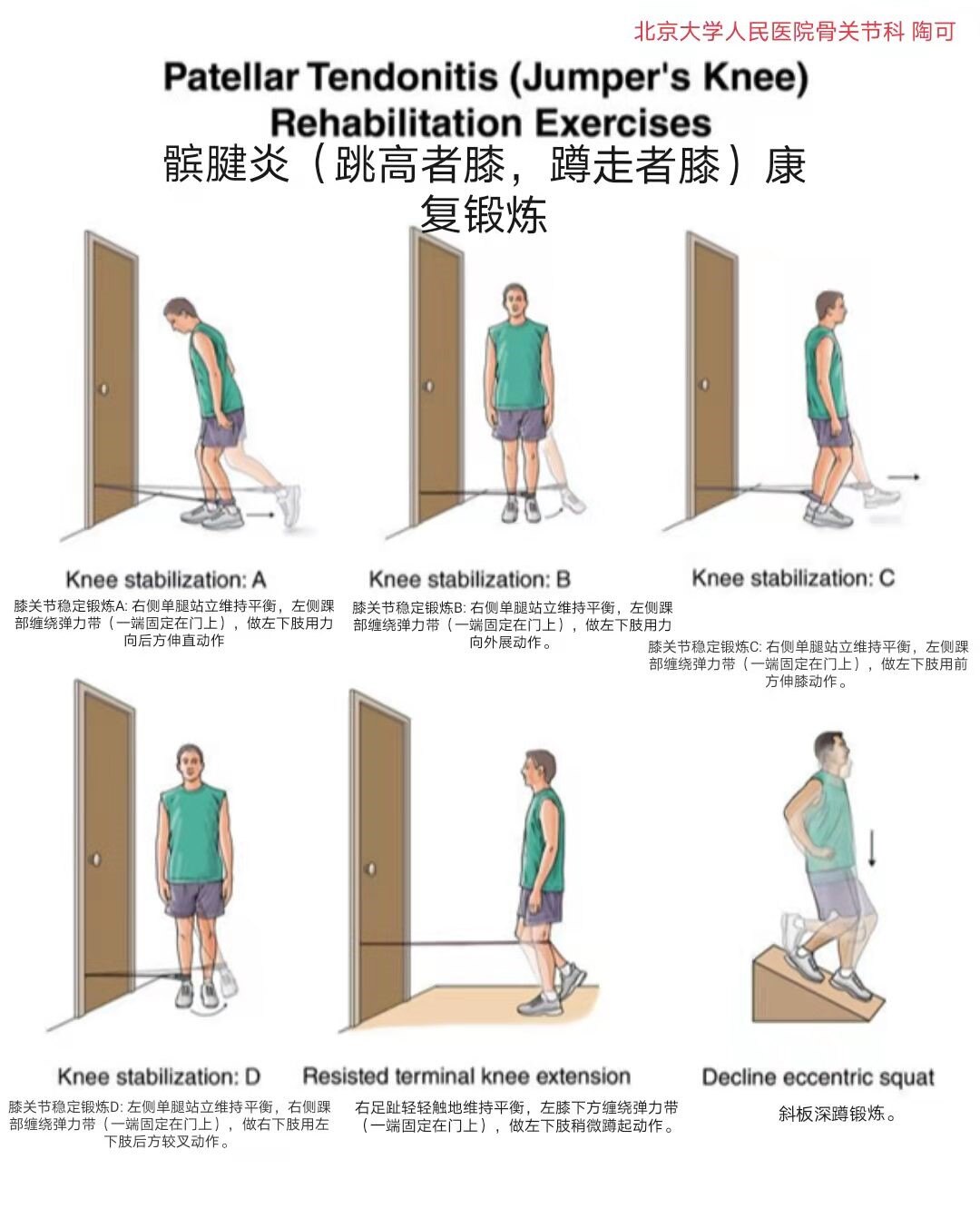
Patellar tendonitis (jumper’s knee) rehabilitation exercises髌腱炎(跳高者膝,蹲走者膝)康复锻炼
Knee stabilization A膝关节稳定锻炼A: 右侧单腿站立维持平衡,左侧踝部缠绕弹力带(一端固定在门上),做左下肢用力向后方伸直动作。
Knee stabilization B膝关节稳定锻炼B: 右侧单腿站立维持平衡,左侧踝部缠绕弹力带(一端固定在门上),做左下肢用力向外展动作。
Knee stabilization C膝关节稳定锻炼C: 右侧单腿站立维持平衡,左侧踝部缠绕弹力带(一端固定在门上),做左下肢用前方伸膝动作。
Knee stabilization D膝关节稳定锻炼D: 左侧单腿站立维持平衡,右侧踝部缠绕弹力带(一端固定在门上),做右下肢用左下肢后方较叉动作。
Resisted terminal knee extension: 右足趾轻轻触地维持平衡,左膝下方缠绕弹力带(一端固定在门上),做左下肢稍微蹲起动作。
Decline eccentric squat斜板深蹲锻炼。

Spanish squats, isometric leg extensions, and leg presses are fantastic exercises for patellar tendonitis.
西班牙深蹲、等长大腿(股四头肌)伸展和下肢推举都是治疗髌腱炎的绝佳练习。
髌腱病是一种常见的肌肉骨骼疾病,其特征是进行性与活动相关的膝前疼痛和髌腱功能障碍。它在涉及跑步和跳跃的运动中非常普遍。髌腱病的治疗中使用了各种治疗方法,包括休息、运动调整、非甾体消炎药物(止疼片)、注射疗法、膏药贴敷、偏心运动、体外冲击波疗法、经皮电疗和手术治疗。尽管髌腱病有多种治疗方案可供选择,但没有一种方法被证明可以使患者持续且接近完全康复。保守治疗被认为是一线治疗。本研究概述了髌腱病治疗的当前实践,重点是康复。这篇综述可以作为运动医学和康复专业人员在这种疾病治疗中的决策指南。
介绍
髌腱病(PT)也称为跳高者膝,常见于涉及跑步和跳跃的运动中[1]。这种肌肉骨骼疾病的特征是进行性与运动相关的膝前疼痛和髌腱功能障碍[2]。这种疾病可能导致运动员和非运动员的残疾,可能影响运动表现,并可能损害职业运动员的运动生涯。高达45%的优秀跳跃运动员和14%的休闲跳跃运动员在任何特定时间都会出现髌腱病(PT)症状[3]。精英篮球运动员和排球运动员的髌腱病(PT)患病率分别为45%和32%[3]。Cook、Khan、Harcourt、Grant、Young、Bonar[4]报告说,超过三分之一的髌腱病(PT)患者在受伤后六个月内无法恢复体育活动。一项前瞻性随访研究[5]报告称,超过50%的髌腱病(PT)运动员被迫退出积极运动。最近的另一项研究6还发现,只有46%髌腱病(PT)运动员在12个月的监督康复后能够恢复到完全活动水平而没有疼痛。
腘绳肌和股四头肌紧绷、踝关节背屈减少、足部过度旋前、关节协调性差、超重、下肢长度差异、训练量和跳跃训练强度增加以及活动量增加是髌腱病(PT)的一些常见危险因素[7-10]。在硬地球场和人造草坪上训练会增加受伤的风险。典型的放射学表现包括髌腱增厚和腱后缘异常[11,12]。髌腱病(PT)的病因尚不完全清楚,这使得治疗方案仍有争议。
各种类型的治疗用于髌腱病(PT)的治疗。这些包括休息、活动调整、非甾体抗炎药物、注射疗法、贴扎、离心运动、体外冲击波疗法、经皮电疗和手术。尽髌腱病(PT)有多种治疗选择,但没有一种方法被证明可以使患者持续且接近完全康复。保守治疗被认为是髌腱病(PT)的一线治疗,采用药物和物理治疗的形式。活动调整应包括减少肌腱负荷的体积和频率。必须纠正涉及腘绳肌和股四头肌的力量不平衡以及柔韧性差,以避免在步行、跑步、跳跃和其他体育活动中偏离正确的生物力学。
药物治疗
文献中关于非甾体抗炎药(NSAID)在髌腱病(PT)中的有效性的非结论性证据[13]。非甾体抗炎药(NSAID)因其镇痛作用而常用于髌腱病(PT)。一些研究报道了非甾体抗炎药(NSAID)对急性髌腱病(PT)的有益作用[14,15]。然而,从长远来看,它可能会对肌腱愈合产生负面影响[16]。Almekinders[17]和Vogel[18]也不支持使用非甾体抗炎药(NSAID),因为它们在肌腱中的有害机制。肌腱周围和肌腱内注射也用于治疗髌腱病(PT)。富含血小板的血浆、皮质类固醇、抑肽酶和透明质酸是促进肌腱愈合最常用的注射剂[19]。各种研究报告了PRP注射对髌腱病的有益作用[20,21]。然而,由于缺乏高质量的研究和程序的不一致,很难对其有效性做出结论[19]。van Ark、Zwerver、van den Akker-Scheek[22]对注射治疗在髌腱病(PT)管理中的有效性进行的系统评价显示出有希望的结果。然而,该领域缺乏高质量的研究。
康复方案
康复的主要目的是通过首先解决疼痛减轻,然后进行渐进性负荷来发展肌腱部分的负荷耐受性。重度慢阻、离心和等长运动用于髌腱病(PT)的康复。研究表明,偏心运动是髌腱病(PT)管理中最有效和最常用的干预策略之一。几位研究人员报告了在髌腱病(PT)中进行偏心锻炼的有效性,症状的长期和短期改善。这样的练习可以增强肌腱内胶原纤维的重塑[1]。这导致肌腱单位适应身体活动引起的压力。在运动和非运动人群中都报告了出色的结果。Larsson、K?ll、Nilsson-Helander[23]对RCT进行的系统评价报告了在髌腱病(PT)管理中使用偏心训练的有力证据。在髌腱病(PT)中使用了几种类型的偏心加载方法。在一项为期12周的前瞻性研究中,Frohm、Saartok、Halvorsen、Renstr?m[24]报告说,双侧和单侧下蹲对髌腱病(PT)的管理同样有效。Purdam、Jonsson、Alfredson、Lorentzon、Cook、Khan[25-27]还断言,与其他管理方法相比,偏心式下蹲深蹲在减轻髌腱病(PT)症状方面的优势。在一篇批判性评论中,Visnes, Bahr[28]证实了离心下蹲的有效性。作者建议深蹲应该在一定难度下进行[28]。Purdam、Cook、Hopper、Khan、Group[29]比较了标准深蹲训练和离心深蹲训练对髌腱病(PT)患者的效果。在接受过偏心训练的8名运动员中,有6名能够重返运动项目,而标准化深蹲样本中只有一名运动员能够重返他们的运动项目。Cannell、Taunton、Clement、Smith、Khan[30]在一项为期12周的随访研究中比较了深蹲和腿弯举的疗效,并报告说这两种治疗方法在减轻髌腱病(PT)症状方面同样有效。据报道,70%的髌腱病(PT)患者接受了精心设计的康复计划,结果非常好。该康复计划的主要组成部分涉及膝关节的开放式动力学链偏心训练[31]。在一项对66名接受偏心训练治疗的髌腱病(PT)患者的回顾性研究中,研究人员报告说,20名患者的疼痛和其他症状完全缓解,42名患者的症状明显改善[32]。同时,在竞技赛季中接受过偏心下蹲训练的排球运动员的症状也出现了恶化[28]。Fredberg、Bolvig、Andersen[33]还报告了在丹麦超级联赛球员中使用赛季内偏心练习后的不利影响和受伤风险增加。这些报告表明,在球员处于高负荷环境时增加偏心负荷会对肌腱产生负面影响。作为康复计划的一部分,正在接受偏心锻炼的运动员建议充分休息。
据报道,负重慢速等张运动可导致疼痛和其他症状的长期和短期改善[30,34,35]、病理学改善[34]、纤维重塑增强[34]和正常化肌腱纤维的形态[36]。尽管与负重慢速抗阻运动相关的结构和可观察到的变化,但大多数支持管理髌腱病(PT)的证据是从患者报告的结果和临床检查中获得的,而不是观察到的结构变化[37]。为期4周的季节性负重慢速等张训练计划改善了髌腱病(PT)运动员的疼痛[38]。这种训练可以恢复肌肉体积和下肢力量,并且可以以最小的疼痛进行[39]。这些练习包括单腿坐姿膝关节伸展、髋关节伸展和髋关节器械外展、小腿抬高等。练习可以以最小的负荷开始,随着症状的进展通过增加负荷来进行。Kongsgaard、Kovanen、Aagaard、Dossing、Hansen、Laursen、Kaldau、Kjaer、Magnusson[34]比较了髌腱病(PT)患者的类固醇注射、离心运动和负重慢速抗阻运动。尽管在12周的随访后所有三种治疗方法的症状都有改善,但只有偏心和缓慢的阻力运动在6个月后显示VISA P评分和VAS量表有所改善。在长期和短期随访中,负重慢速阻力运动显示出组织正常化的改善,并报告了比其他方法更好的临床表现。与偏心训练计划(22%)相比,负重慢速阻力运动计划的患者满意度显着提高(70%)。在比较各种负荷计划的系统评价中,Malliaras、Barton、Reeves、Langberg[40]建议在髌腱病(PT)管理中采用一种包括同心和偏心训练计划的组合方法。Silbernagel、Thomeé、Eriksson、Karlsson[41]还推荐了一种综合方法,包括髌腱病(PT)管理中的偏心、向心和增强式训练计划。
康复阶段
提出的三阶段康复方案是基于作者的最新研究和意见。该协议可以指导临床医生在髌腱病(PT)患者的运动进展中。未提及运动剂量,因为它可能会因个人因素而异。
第1阶段:疼痛调节和负荷管理:康复的初始阶段应侧重于负荷管理和疼痛调节,特别是对于赛季中的运动员。在这个阶段必须解决下肢的生物力学损伤,例如力量不平衡和柔韧性差。负荷管理和活动量调整是减轻髌腱病(PT)疼痛和其他症状的一些最有效的方法[2]。然而,避免完全停止活动也很重要,因为这可能会进一步降低肌腱的负荷能力。减少训练的量和频率,从训练中去除高负荷的能量储存活动,如跑步、跳跃等,是肌腱负荷管理的一些最有效的方法。研究表明,持续的中程等长运动是减轻髌腱病(PT)疼痛的有效方法。一项交叉研究[42]和一项随机对照试验38报道了等长运动对髌腱疼痛的显着急性影响。Rio、Purdam、Girdwood、Cook[43]最近进行的一项实用临床试验表明,为当季运动员提供的等长下蹲运动可以减少不同运动和时间表的疼痛。根据Rio、Kidgell、Purdam、Gaida、Moseley、Pearce、Cook[42]的说法,在腿部伸展机上进行5次重复45秒的股四头肌等长运动,可以在髌腱病(PT)患者中诱导数小时的镇痛。当健身器材的使用受限时,在固定在小腿上的弹性带的支撑下,具有70-90度膝盖弯曲角度的西班牙深蹲可能是一种替代方式[44]。
第2阶段:加强锻炼和负荷进展:一旦患者能够以最小的疼痛进行等张运动,就可以开始重度慢速抗阻运动和离心运动[7]。Kongsgaard、Kovanen、Aagaard、Dossing、Hansen、Laursen、Kaldau、Kjaer、Magnusson[34]之前曾提出过一种用于髌腱病(PT)的重度慢速阻力练习方案,该方案包括从膝关节伸展到膝关节90°的深蹲、后蹲和腿举屈曲。以前的研究报道了负重慢阻力训练和偏心运动的有益效果[28,29,34,45]。负重慢速抗阻运动可以增强肌腱的力学性能,并可能导致肌腱肥大[45]。建议逐步进行练习。随着病情的进展,可以进行涉及单肢的锻炼。可以通过加重的腰带、背心或带重量的袋子来提供额外的阻力。
第3阶段:功能强化和恢复运动:功能强化的主要重点是运动模式和动力链缺陷,以及高负荷肌腱能力。一旦运动模式和动力学链得到改善,训练就可以进行到增强式和特定运动的活动。高能训练,如跳跃、跳跃和短跑,以及弹跳动作和敏捷性训练也应包括在训练计划中。所有的训练和负荷都必须进行监控和量化,对于重新引入高负荷活动,建议采用高-低中负荷日方法。预后和恢复运动的决定因素是疼痛严重程度、病理和功能障碍。
其他干预
其他常用的髌腱病(PT)干预措施有冰敷疗法、肌筋膜松解、横向摩擦按摩、绑扎和支撑等[13]。冰敷疗法可用于缓解疼痛,但不建议在比赛或训练之前使用,因为它可能掩盖疼痛并最终导致新的伤害[46]。尽管文献没有提供太多证据,但脉冲超声也被用作治疗髌腱病(PT)的一种治疗方式[47]。van Leeuwen、Zwerver、van den Akker-Scheek[48]的系统评价得出结论,体外冲击波治疗(ECSWT)可以在髌腱病(PT)管理中提供有希望的结果。同时,Zwerver、Hartgens、Verhagen、van der Worp、van den Akker-Scheek、Diercks[49]没有找到ECSWT对髌腱病(PT)运动员的任何有益作用。van der Worp、van den Akker-Scheek、van Schie、Zwerver[50]认为,ECSWT可以通过对疼痛区域的过度刺激来减少疼痛信号向大脑的传递,可以支持肌腱的组织再生,并且可以破坏组织钙化。反贴和支撑可以通过纠正髌骨和髌腱之间的角度来减少髌骨应变[51]。
手术管理
绝大多数患者对保守治疗有积极反应。然而,如果保守治疗失败,一些进展到手术治疗。关节镜检查和开放手术都是常用的。在监督康复后,恢复体育活动的平均时间可能为3到9个月不等[13]。根据Brockmeyer、Diehl、Schmitt、Kohn、Lorbach[52]的研究,开放手术和关节镜手术的成功率分别为87%和91%。同时,与关节镜检查(平均3.9个月)相比,开放手术恢复体育活动需要更长的时间(平均8.3个月)[52]。两种手术方法的平均运动恢复率相似。两种手术技术的术后康复程序几乎相似,包括疼痛调节、离心锻炼和加强计划。文献中没有关于使用一种技术优于另一种技术的明确指南。关节镜技术是最常见的,因为它可以更快地恢复运动。
术后康复可以在拐杖部分负重开始(术后第1天)[53]。非负重全方位运动练习可以在早期阶段开始。随着患者病情的改善,可以进行轻度向心和偏心运动(术后5-7天)和肌腱负荷(术后7-14天)[53,54]。最大负荷活动可以在手术后两周开始。
髌腱病(PT)伤害预防
关于预防髌腱病(PT)的文献有限。髌腱病(PT)中最常用的预防方法是静态拉伸、核心稳定性练习、足部矫形器、减震鞋垫和女性激素替代疗法[55]。足球专项平衡训练可以减少肌腱病变,训练持续时间与损伤发生率之间存在剂量效应关系[56]。Fredberg、Bolvig、Andersen[33]报告说,预防性偏心运动和下肢肌肉拉伸可以防止肌腱异常的发展。然而,对受伤风险没有积极影响。建议进一步研究预防髌腱病。
结论
髌腱病是一种肌肉骨骼疾病,主要见于涉及由跑步和跳跃组成的活动的运动中。尽管有多种治疗方案可供选择,但髌腱病(PT)的管理仍存在争议。保守治疗是最优选的治疗方法,包括疼痛调节、负荷管理、负荷进展和功能强化。这种康复的目的是通过首先解决疼痛减轻,然后进行渐进性负荷来发展肌腱部分的负荷耐受性。
Rehabilitation of patellar tendinopathy
Abstract
Patellar tendinopathy is a common musculoskeletal disorder characterized by progressive activity-related anterior knee pain and patellar tendon dysfunction. It is highly prevalent in sports which involve running and jumping. Various treatment methods are used in the management of PT including rest, activity modification, anti-inflammatory medication, injection therapies, taping, eccentric exercises, extra corporeal shock wave therapy, percutaneous electrolysis, and surgery. Even though various treatment options are available for patellar tendinopathy, no single method has proven to result in a consistent and near complete recovery in patients. Conservative management is considered to be the first line of treatment. This study presents an overview of the current practice about the management of patellar tendinopathy with an emphasis on rehabilitation. This review can act as a guide to sports medicine and rehabilitation professionals‘ decision making in the management of this disorder.
Introduction
Patellar tendinopathy (PT) which is also known as jumpers’ knee is commonly seen in sports which involve running and jumping[1]. This musculoskeletal disorder is characterized by progressive activity-related anterior knee pain and patellar tendon dysfunction[2]. This disorder can lead to disability in both athletes and non-athletes, may impact on athletic performance, and may impair the athletic career of professional players. Up to 45% of elite jumping athletes and 14% of recreational jumping athletes experience the symptoms of PT at any given time[3]. The prevalence of PT among elite basketball and volleyball players is 45% and 32% respectively[3]. Cook, Khan, Harcourt, Grant, Young, Bonar[4] reported that more than one-third of the patients who presented with PT were not able to return to sports activities within six months following injury. A prospective follow-up study[5] reported that more than 50% of athletes with PT were forced to retire from active sport. Another recent study6 also found that only 46% of athletes with PT were able to return to full activity level with no pain following 12 months of supervised rehabilitation.
Hamstring and quadriceps muscle tightness, reduced ankle dorsiflexion, hyper pronation of the foot, poor joint coordination, being overweight, leg length discrepancy, increased training volume and intensity of jump training and greater activity volume are some of the common risk factors for PT[7-10]. Training on hard courts and synthetic turf can increase the risk of injury. The typical radiological finding includes thickening of the patellar tendon and abnormalities in the posterior border of the tendon[11,12]. The etiopathology of PT is not fully understood, which makes the treatment options still controversial.
Various types of treatment are used in the management of PT. These include rest, activity modification, anti-inflammatory medication, injection therapies, taping, eccentric exercises, extra corporeal shock wave therapy, percutaneous electrolysis, and surgery. Even though various treatment options are available for PT, no single methods has proven to result in consistent and near complete recovery in patients. Conservative management is considered to be the first line of treatment in PT, in the form of medical and physical therapies. Activity modification should involve reducing the volume and frequency of load on the tendon. Strength imbalances involving hamstring and quadriceps muscles, as well as poor flexibility, must be corrected to avoid deviation from correct biomechanics during walking, running, jumping and other sporting activities.
Medical therapy
Non-conclusive evidence is available in the literature regarding the effectiveness of non-steroidal anti-inflammatory drugs (NSAID) in PT[13] . NSAID are commonly used in PT due to their analgesic effect. The beneficial effects of NSAID in acute PT has been reported in some studies[14,15]. However, it may negatively affect tendon healing in the long-term[16]. Almekinders[17] and Vogel[18] also does not support the use of NSAIDS due to their deleterious mechanism in the tendon. Peri-tendinous and intra-tendinous injections are also used in the treatment of PT. Platelet-rich plasma, corticosteroids, aprotinin and hyaluronic acid are the most commonly used injections for the promotion of tendon healing[19]. Various studies reported beneficial effects of PRP injection on patellar tendinpaothy[20,21]. However due to lack of high quality researches and inconsistency in procedures makes it difficult to draw a conclusion on its effectiveness[19]. A systematic review by van Ark, Zwerver, van den Akker-Scheek[22] on the effectiveness of injection treatment in the management of PT showed promising results. However, there is a paucity of high-quality research in this area.
Rehabilitation protocol
The key aim of rehabilitation is to develop load tolerance on the part of the tendon by addressing pain reduction initially, followed by progressive loading. Heavy slow resistance, eccentric and isometric exercises are used in the rehabilitation of PT. Studies reveal that eccentric exercise is one of the most effective and commonly-used intervention strategies in the management of PT. Long-term and short-term improvement in symptoms were reported by several researchers into the effectiveness of eccentric exercises in PT. Such exercises can augment the remodeling of collagen fibers within the tendon[1]. This leads to the musculotendinous unit adapting itself from stress resulting from physical activity. Excellent results have been reported in both athletic and non-athletic populations. Strong evidence for the use of eccentric training in the management of PT was reported in a systematic review of RCTs conducted by Larsson, K?ll, Nilsson-Helander[23]. Several types of eccentric loading methods are used in PT. In a 12 week prospective study, Frohm, Saartok, Halvorsen, Renstr?m[24] reported that both bilateral and unilateral decline squats were equally effective in the management of PT. Purdam, Jonsson, Alfredson, Lorentzon, Cook, Khan[25-27] also asserted the supremacy of eccentric decline squats compared with other management methods in reducing the symptoms of PT. In a critical review, Visnes, Bahr[28] confirmed the effectiveness of eccentric decline squats. The authors suggested that the squat should be performed at certain levels of difficulty[28]. Purdam, Cook, Hopper, Khan, Group[29] compared the effectiveness of standard squat training and eccentric squat training in patients with PT. Six out of eight athletes who had undergone eccentric training were able to return to sports participation, whereas only one athlete from the standardized squat sample were able to return to their sport. Cannell, Taunton, Clement, Smith, Khan[30] compared the efficacy of drop squats with leg curls in a 12-week follow-up study, and reported that both treatment methods were equally effective in reducing symptoms of PT. An excellent outcome was reported in 70% of patients with PT who underwent a well-designed rehabilitation program. The major component of this rehabilitation program involved open kinetic chain eccentric training of the knee[31]. In a retrospective study of 66 PT patients treated with eccentric training, the researchers reported a complete relief of pain and other symptoms in 20 patients, and a marked improvement in symptoms in 42 patients[32]. At the same time, there was a worsening of the symptoms in volleyball players who had received eccentric decline squat training during the competitive season[28]. Fredberg, Bolvig, Andersen[33] also reported a detrimental effect and increased risk of injury following the use of in-season eccentric exercises among Danish super league players. These reports suggest that addition of eccentric loading while the players is in a high loading environment can have a negative impact on the tendon. Adequate rest is advised for athletes who are undergoing eccentric exercising as part of a rehabilitation program.
Heavy slow isotonic exercises have also been reported as leading to long-term and short-term improvement in pain and other symptoms[30,34,35], improvement in pathology[34], augmentation in the remodeling of fibers[34] and normalization of the morphology of tendon fibrils[36]. Even though there are structural and observable changes associated with heavy slow resistance exercises, most of the evidence supporting managing PT is obtained from patient reported outcomes and clinical examinations rather than observed structural changes[37]. A four-week in-season heavy slow isotonic training program resulted an improvement in pain in athletes with PT[38]. Such training can restore muscle bulk and the strength of the lower extremity, and can be performed with minimal pain[39]. These exercises include single leg seated knee extensions, hip extensions and abduction with hip machines, calf raises, etc. The exercise can be started with a minimal load and progress by increasing load as the symptoms progress. Kongsgaard, Kovanen, Aagaard, Doessing, Hansen, Laursen, Kaldau, Kjaer, Magnusson[34] compared steroid injections, eccentric exercise, and heavy slow resistance exercise in patients with PT. Even though there was improvement in symptoms in all the three treatment methods after 12-weeks of follow-up, only eccentric and slow resistance exercise showed improvement in the VISA P score and the VAS scale after six months. The heavy slow resistance exercise showed an improvement in tissue normalization and reported a better clinical presentation than the other methods in both long-term and short-term follow ups. Patient satisfaction was found to be significantly higher (70%) in the heavy slow resistance exercise program when compared to the eccentric training program (22%). In a systematic review which compared various loading programs, Malliaras, Barton, Reeves, Langberg[40] recommended a combined approach involving both concentric and eccentric training programs in the management of PT. Silbernagel, Thomeé, Eriksson, Karlsson[41] also recommended a combined approach including eccentric, concentric, and plyometric training programs in the management of PT.
Stages of rehabilitation
The proposed three-stage rehabilitation protocol is based on latest researches and opinion of the author . This protocol can guide the clinician in the exercise progression of PT patients. The exercise dosage is not mentioned as it may vary, based on individual factors.
Stage 1: Pain modulation and load management: The initial stages of rehabilitation should focus on load management and pain modulation, especially in the case of in-season athletes. Biomechanical impairment of the lower extremities such as strength imbalance and poor flexibility must be addressed at this stage. Load management and activity modification are some of the most effective methods to reduce pain and other symptoms of PT[2]. However, it is also important to avoid the complete cessation of activities as this may further reduce the loading capacity of the tendon. Reducing the volume and frequency of training, removing high load energy storage activities such as running, jumping etc. from the training are some of the most effective methods for the load management of the tendon. Studies shows that sustained mid-range isometric exercise is an effective method of pain reduction in PT. Substantial acute effect of isometric exercise on patellar tendon pain was reported in a cross-over study[42] and in a randomized control trial38. A recent pragmatic clinical trial conducted by Rio, Purdam, Girdwood, Cook[43] demonstrated that an isometric squat exercise offered to in-season athletes reduces pain across different sports and schedules. According to Rio, Kidgell, Purdam, Gaida, Moseley, Pearce, Cook[42] five repetitions of 45-second isometric quadriceps exercises on a leg extension machine induces analgesia for several hours in patients with PT. A Spanish squat with 70-90 degree knee flexion angle with the support of a rigid strap fixating at the lower leg can be an alternative way when there is a limited access to gym equipment[44].
Stage 2: Strengthening exercises and load progression: Once the patient can perform isotonic exercise with minimal pain, heavy slow resistance exercises and eccentric exercises can be initiated[7]. An heavy slow resistance exercises protocol for PT has previously been suggested by Kongsgaard, Kovanen, Aagaard, Doessing, Hansen, Laursen, Kaldau, Kjaer, Magnusson[34] which consists of squat, hack squat and leg press from knee extension to 90o of knee flexion. The beneficial effects of heavy slow resistance training and eccentric exercises are reported in previous studies[28,29,34,45]. Heavy slow resistance exercise can augment tendon mechanical properties and can cause hypertrophy of the tendon[45]. A gradual progression of the exercises are recommended. Exercises involving a single limb can be performed as the condition progresses. Additional resistance can be provided by means of weighted belts, vest or bags with weight.
Stage 3: Functional strengthening and return to sports: The major focus of functional strengthening is on movement pattern and kinetic chain deficits, as well as on the high load tendon capacity. Once the movement pattern and kinetic chain is improved the training can progress to plyometric and sport-specific activities. High energy training such as skipping, jumping and sprinting, and bounding movements and agility training should also be included in the training program. All the training and loading must be monitored and quantified, and a high -low medium load day approach is recommended with regard to the re-introduction of high-load activities. The determinants of prognosis and return to sport are pain severity, pathology, and dysfunction.
Other interventions
Other commonly-used interventions for PT are cryotherapy, myofascial release, transverse friction massage, taping and bracing, etc.[13]. Cryotherapy can be used for pain relief but cannot be recommended prior to competition or training as it may mask the pain and ultimately lead to a new injury[46]. Even though the literature doesn’t provide much evidence, pulsed ultra sound has also been used as a therapeutic modality for the management of PT[47]. A systematic review by van Leeuwen, Zwerver, van den Akker-Scheek[48] concluded that extra-corporeal shock wave therapy (ECSWT) can provide promising results in the management of PT. At the same time, Zwerver, Hartgens, Verhagen, van der Worp, van den Akker-Scheek, Diercks[49] did not find. any beneficial effect of ECSWT in athletes with PT. According to van der Worp, van den Akker-Scheek, van Schie, Zwerver[50], ECSWT can diminish the transmission of pain signals to the brain by hyper-stimulation of the painful area, can support tissue regeneration of the tendon, and can destroy tissue calcification. Counter-taping and bracing can reduce patellar strain by correcting the angle between the patella and the patellar tendon[51].
Surgical management
A vast majority of patients positively respond to conservative treatment. However, a few progresses to surgical management if conservative management fails. Both arthroscopy and open surgery are commonly used. The average time period for return to sports activities may vary from 3 to 9 months following a supervised rehabilitation[13]. According to Brockmeyer, Diehl, Schmitt, Kohn, Lorbach[52], the success rate of open and arthroscopic surgeries are 87% and 91% respectively. At the same time, return to sports activities takes longer (8.3 months on average) in the case of open surgery compared to in the case of arthroscopy (3.9 months on average)[52]. The average rate of return to sports are similar in both surgical methods. The post-operative rehabilitation procedures for both surgical techniques are almost similar, and includes pain modulation, eccentric exercises and strengthening programs. There are no clear guidelines available in the literature about the use of one technique over another. The arthroscopic technique is most-commonly preferred due to its leading to a faster return to sport.
Post-operative rehabilitation can be initiated with partial weight bearing in crutches (day 1- post surgery)[53]. Non weight bearing full range of motion exercises can be started at earlier stages. Light concentric and eccentric exercises (5-7 days post-surgery) and tendon loading can be progressed (7-14days post-surgery) as the patient improves his condition[53,54]. Maximal loading activity can be started two weeks post-surgery.
Injury prevention
There is a limited literature available regarding the prevention of PT. The most common preventive methods used in PT are static stretching, core stability exercises, foot orthosis, shock absorption insoles and hormone replacement therapy in females[55]. Soccer-specific balance training can reduce tendinopathy with a dose effect relationship between the duration of training and the incidence of injury[56]. Fredberg, Bolvig, Andersen[33] reported that prophylactic eccentric exercises and stretching of the lower limb muscles can prevent the development of tendon abnormalities. However, there was no positive impact on risk of injury. Further research is recommended regarding the prevention of patellar tendinopathy.
Conclusion
Patellar tendinopathy is a musculoskeletal condition predominantly seen in sports which involve activities made up of running and jumping. Even though several treatment options are available, the management of PT is still controversial. Conservative management is the most preferred method of treatment and includes pain modulation, load management, load progression and functional strengthening. The aim of such rehabilitation is to develop load tolerance on the part of the tendon by addressing pain reduction initially, followed by progressive loading.
文献出处:Qassim I Muaidi. Rehabilitation of patellar tendinopathy. Review, J Musculoskelet Neuronal Interact. 2020 Dec 1;20(4):535-540.
图片来源Google images,https://martinkoban.com/patellar-tendonitis-treatment/
本文是陶可版权所有,未经授权请勿转载。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论