 三甲
三甲
骨软骨损伤:所有软骨疾病都是一样的情况?
骨软骨损伤:所有软骨疾病都是一样的情况?
Are all Cartilage Problems the Same?
陶可(北京大学人民医院骨关节科)
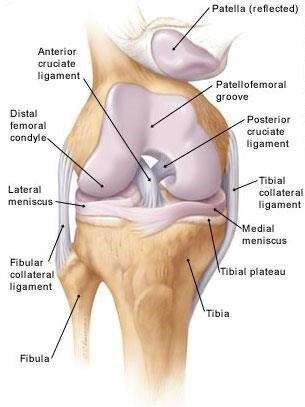
图1. 正常膝关节是由髌骨(patella)、股骨(patellofemoral groove、distal femoral condyle)、胫骨(tibia)(腓骨,fibula)以及前交叉韧带(anterior cruciate ligament)、后交叉韧带(posterior cruciate ligament)、半月板(lateral meniscus、medial meniscus)以及内侧副韧带(tibial collateral ligament)、外侧副韧带(fibular collateral ligament)组成人体最复杂的且最容易发生损伤的关节。
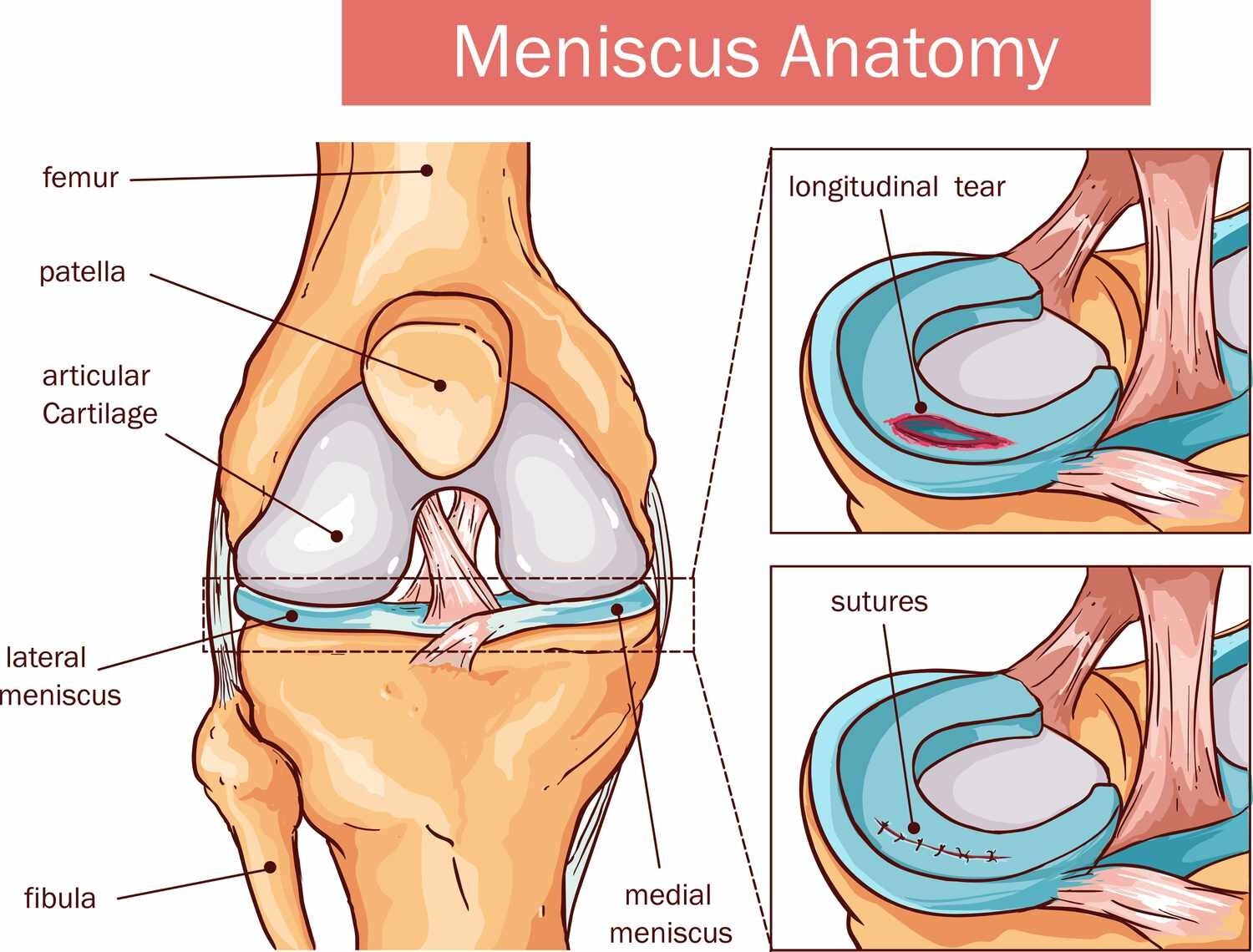
图2. 当膝关节半月板发生撕裂损伤(如longitudinal tear 纵行撕裂)时,早期及时准确的诊断(多采用膝关节核磁共振MRI检查),精确的半月板缝合手术治疗(通常是在关节镜下完成)是最适合的治疗方式,从而避免膝关节发生进一步的软骨损伤以及退行性骨关节炎。
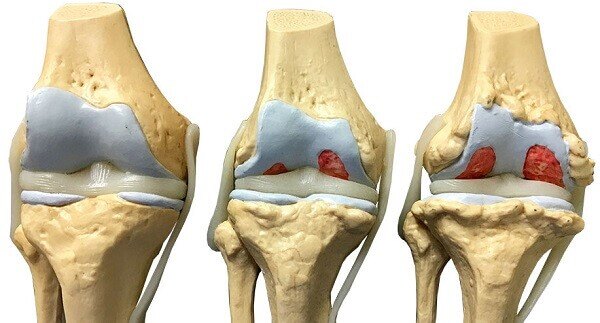
图3. 正常、轻度和重度膝关节软骨损伤的图示。
关节(例如膝关节)由两种类型的软骨形成。第一个关节软骨形成光滑的润滑层,可防止骨骼之间的磨损。第二种是半月板软骨,负责吸收震荡(如跑跳时的冲击力),而不是防止磨损。后一种软骨与骨骼无关,只是充填于在骨骼之间。
关节软骨组织可以通过多种不同方式发生损坏或老化退变,包括:
•外伤(包括运动损伤、意外摔倒、交通事故等);
•反复使用(如爬山、上下楼梯、蹲起练习、跑跳、跷二郎腿等);
•先天性异常;
•软骨疾病。
大多数情况下,“撕裂”是指半月板软骨的损伤,通常比关节软骨受伤要严重得多。这是永久的,并且有长期的并发症。
尽管软骨问题的许多根本原因可能会导致一样或相似的结果(疼痛,身体残疾等),但重要的是要知道软骨问题是多种疾病,具有不同的个人症状和治疗方式。
本节将探讨软骨在各个方面之间的差异,并概述治疗方案和需要考虑的重要因素。
目标受众(阅读者)
本文适用于对关节软骨损害及其家人的任何人群,想了解不同类型的软骨问题以及对软骨问题感兴趣的任何人。
软骨问题的常见类型是什么?
由于多种原因,软骨可以随着时间的流逝而发生老化退变,包括:
•衰老
•肥胖
•跨关节的不平衡力(应力过于集中于关节某处)
•疾病
软骨也可能造成“局灶性”损伤,因此,事故或钝力在关节中造成创伤,进而导致软骨损伤或死亡。
老化退变的软骨问题
诸如骨关节炎之类的疾病会导致软骨随着时间的流逝而发生退行性改变。这会导致骨骼之间产生摩擦,导致疼痛和关节活动度减小。这种类型的软骨损伤可能会在多年内发展。
关于退行性软骨问题的治疗可能包括:
•关节腔内注射凝胶状化合物(例如透明质酸,即玻璃酸钠注射液);
•使用非甾体类抗炎药(NSAIDs,即止疼药)缓解疼痛和炎症;
•被认为有助于重建软骨的饮食补充剂(例如,葡萄糖/软骨素,但2019年国际骨关节炎研究协会和2020中国骨关节炎诊疗指南,都不推荐);
•更保守的方法,例如力量训练和理疗。
变性软骨问题的严重性和长期前景各不相同。但是,减慢或停止退化的进度(缓解疼痛)可以提高患者的生活质量,直到最终可能需要关节置换或其他手术治疗。
治疗取决于关节的类型
虽然许多不同的治疗疗法可用于各种关节和软骨区域,但在某些关节中已经建立了许多治疗方法,而其他地方缺乏数据。
例如,自体软骨细胞植入(ACI) - 在关节镜手术探查过程中,获取了关节软骨组织,在实验室扩增软骨细胞,用以治疗膝关节和踝关节骨软骨损伤病变;但不适合髋关节和肩关节的治疗。
从身体其他部位进行的成功取材软骨也取决于个体因素,包括供体和受体部位的天然软骨的厚度。
年龄,大小和其他因素
使每个软骨问题相对独特的关键因素是每个患者的个人特征和身体情况(如术前、术后体育锻炼强度要求等)。
许多专门针对软骨修复的治疗方式(例如,通过植入细胞或从身体其他区域植入软骨),已经批准用于治疗大约15-55岁患者的骨软骨缺损。
然而,个人情况可能表明,用全关节置换手术将带来更好的结果(因为这是一种更加确定的治疗技术)。在老年患者(可能有限的软骨再生能力)中,尤其是这种情况,并且正处于全关节置换手术是一个更好的选择生活阶段,考虑到他们的疼痛水平和身体生活方式。
相反,在某些情况下,患者对手术方法的风险太大(或无法接受手术治疗的痛苦),可以解决软骨问题的更保守的方式,例如物理疗法等。
软骨损伤的大小也是一个问题。虽然目前的治疗指导尚未完全统一,但修复小的局灶的,局部受损软骨的缺损,通常仅限于直径不超过2 cm的大小。对于处理损伤直径大于此(2 cm),可能需要使用更具侵袭性的方式,以修复整个关节表面的损伤。
然而,一位高大男性的大于2厘米的软骨病变显然比一位娇小女性同样大小的软骨损伤的相对面积较小,因此,医生需要评估每一位患者的软骨损伤问题,以评估该患者的风险和获益,并相应地个体化地制定治疗方案。
患者术后的期望管理和生活质量
目前没有完美的软骨修复的治疗方式。因此,患者需要客观认识并根据自己的软骨伤情等情况,管理术后的期望。软骨病变存在的疼痛和活动受限水平个体差异很大,尽管有些人在运动过程中可能会出现轻微不适,但其他人几乎可能会持续剧烈疼痛。
在这些情况下,软骨修复或手术后的生活质量改善对于事先严重的疼痛和活动受限的患者将更加重要。较小症状的患者往往可能会看到相对较小的术后改善。
从本质上讲,每个患者的病情可能会处在一个变化过程,最终意味着那些从手术中受益最大的人可能会要准备承担更大手术的风险和不适感。
常见问题(常见问题解答)
软骨修复后我可以期待什么样的改善?
这将取决于您的症状的严重程度。治疗前严重且令人无法忍受疼痛的患者,很可能会看到其生活质量明显改善,这将使他们能够重返以前似乎不可能的活动。
那些只有轻度症状的人(例如,只有在跑步时疼痛)可能不会看到当前手术保证干预的好处。在这些情况下,更保守的物理疗法可能更合适。
为什么我不可以使用所有软骨修复方式治疗?
有多种治疗方法可用于修复或更换受损的软骨和关节。但是,软骨损害本身和个体患者情况,都意味着某些方法不太可能使患者受益,因为他们太冒险了,或者不足以更先进更好,无法提供目前的解决方案。
请放心,通常对于大多数类型的软骨损伤都有几种治疗选项,因此请与您的医生联系,以获取最适合您的个体化的解决方案。
Joints, such as the knee, are formed of two types of cartilage. The first, articular cartilage, forms a smooth, lubricating layer that prevents wear between the bones. The second type is the meniscus cartilage, tasked with shock absorption, as opposed to preventing wear and tear. This latter type of cartilage is not connected to the bone; it merely rests between them.
The lubricating tissue that lines the joints, known as cartilage, can be damaged or degraded via a number of different ways, including:
· Injury (including sports accidents)
· Repetitive use
· Congenital abnormalities
· Cartilage disease
Most often, a ‘tear’ refers to an injury of the meniscus cartilage, which is usually much less severe than injury to the articular cartilage. This is permanent, and has long-term complications.
While many of the root causes of cartilage problems may result in similar overall outcomes (pain, physical disability, etc.) it is important to know that cartilage problems are a diverse group of conditions, with different individual symptoms and treatments.
This section will explore the differences – where applicable – between various aspects of cartilage conditions, as well as outlining the treatment options and considerations that might be important to know for your own circumstances.
Intended audience
This article is intended for anyone suffering from damage to their articular cartilage and their families who would like to find out about the different types of cartilage problems, as well as anyone interested in cartilage problems.
What are common types of cartilage problems?
Cartilage can degenerate over time for a number of reasons including:
· Aging
· Obesity
· Unbalanced forces across a joint
· Disease
There can also be ‘focal’ injuries to cartilage, whereby an accident or blunt force causes trauma in a joint that in turn leads to damaged or dead pockets of cartilage.
Degenerative cartilage problems
Conditions such as osteoarthritis cause cartilage to degrade over time. This leads to rubbing between the bones, causing pain and reduced mobility. This type of cartilage damage may develop over many years.
Treatment for degenerative cartilage problems may include:
· The injection of gel-like compounds (e.g., hyaluronic acid)
· Pain and inflammation relief using non-steroidal anti-inflammatory drugs (NSAIDS)
· Dietary supplements that are thought to help rebuild cartilage (e.g. glucosamine/chondroitin)
· More conservative methods such as strength training and physiotherapy
The severity and long-term prospects for degenerative cartilage problems vary. However, slowing or halting the progress of degeneration (with adequate pain relief) can extend a person’s quality of life until, ultimately, a replacement joint or other surgical procedure may be required.
Treatments depend on the type of joint
While many different treatment therapies can be used in a variety of joints and cartilage areas, a number of treatments have become established in certain joints, with data lacking elsewhere.
For instance, autologous chondrocyte implantation (ACI) – in which cartilage cells from the joint are harvested, multiplied in a laboratory and then replanted in the joint at much higher concentrations – is established for the knee and ankle, but is less appropriate for the hip and shoulder joints.
Successful cartilage grafting from other parts of the body will also depend on individual factors, including the thickness of the natural cartilage at both the donor and recipient sites.
Age, size and other factors
A crucial factor that makes every cartilage problem relatively unique is the individual characteristics and circumstances of each patient.
Many treatment options that focus specifically on the repair of cartilage (by implanting cells or grafting cartilage from other areas of the body, for example) are approved for patients aged approximately 15–55 years.
Nevertheless, individual circumstances may suggest that a total joint replacement with a synthetic implant will give a better outcome (as this is a more established technique). This is particularly the case in older patients, who may have limited cartilage regeneration abilities, and are at a stage in their lives where the decision to take on a synthetic joint is a better choice, given their level of pain and physical lifestyle.
Conversely, it may be in some cases that patients are considered too risky for surgical approaches, and more conservative management of cartilage problems can be pursued, such as physiotherapy.
The size of the cartilage damage is also an issue. While current guidelines are not set in stone, the repair of small focal, localised pockets of damaged cartilage is often limited to a size roughly no more than 2 cm in diameter. Damaged areas larger than this may need to be treated as part of the whole surface of the joint using more aggressive strategies.
Nevertheless, a 2 cm lesion on a large male is clearly relatively smaller than one of a similar size in a petite female, so individual cartilage problems need to be assessed by a physician to gauge the risks and benefits for that patient, and tailor treatment accordingly.
Managing expectations, and quality of life
There is currently no perfect cartilage repair treatment. Patients therefore need to manage their expectations to their individual circumstances. The level of pain and immobility present in cartilage problems varies widely, and while some people may have mild discomfort during athletic pursuits, others may be in severe pain almost continuously.
In these situations, quality of life improvements following cartilage repair or surgery will be much more significant in patients who had crippling pain and immobility beforehand. Patients with only minor symptoms may see relatively little benefit, especially when factoring in the disruption surgery can have in their lives.
In essence, each patient will be on a sliding scale that will ultimately mean those who stand to benefit the most from a procedure may feel more ready to take on the risks and discomforts of surgery.
Frequently Asked Questions (FAQs)
What improvement can I expect following cartilage repair?
It will depend on the severity of your symptoms beforehand. Patients with severe and debilitating pain prior to treatment will most likely see a marked improvement in their quality of life that will allow them to return to activities that may have previously seemed impossible.
Those with only mild symptoms (for instance, pain only when running) may not see enough benefit from current procedures to warrant intervention. In these cases, more conservative physical therapy may be more appropriate.
Why aren’t all the cartilage repair options available to me?
There are a multitude of treatments available to either repair or replace damaged cartilage and joints. However, both the cartilage damage itself, and individual patient circumstances, means that some approaches are either unlikely to benefit the patient because they are are too risky or are not advanced enough to offer a solution at the present time.
Rest assured there are usually several options for most types of cartilage complaints, so speak to your physician for a tailored solution appropriate to you.
Further reading
· A Primer in Cartilage Repair and Joint Preservation of the Knee. Editor: Minas T. 2011: Elsevier. ISBN 978-1-4160-6654-5
· Articular Cartilage Lesions. A Practical Guide to Assessment and Treatment. Editors: Cole B, Malek, M. 2004: Springer Verlag New York. ISBN 0-387-95540-2
· Cartilage Surgery: An Operative Manual. Editors: Brittberg M, Gersoff W. 2011: Saunders/Elsevier ISBN: 978-1-43770878-3
Keywords
Cartilage, cartilage repair, quality of life
关键词
软骨,软骨修复,生活质量
本文是陶可版权所有,未经授权请勿转载。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论