 三甲
三甲
AMIC Chondro-Gide软骨基质I/III型胶原纤维支架联合微骨折技术修复膝关节软骨缺损2
AMIC Chondro-Gide 软骨基质I/III型胶原纤维支架联合微骨折技术修复膝关节软骨缺损2
2个手术案例
自体基质诱导的软骨再生(Autologous matrix-induced chondrogenesis, AMIC)手术是一步法修复软骨缺损的技术。在关节镜下评估软骨损伤并决定进行 AMIC 手术后,进行微创膝关节切开术。用于修复膝关节软骨缺损的全关节镜 AMIC 手术已经报道。 [4]
Autologous Matrix Induced Chondrogenesis (AMIC) surgery is a single step procedure. After arthroscopic evaluation of the cartilage damage and decision for an AMIC procedure a mini arthrotomy is performed. An all-arthroscopic AMIC procedure for repair of cartilage defects of the knee is also possible.[4]
首先,暴露并清理成形原软骨缺损,目的是小心去除所有不稳定的退化软骨,包括钙化的软骨下层。然后,使用无菌可压模材料(例如铝箔)获取缺陷的印记(尺寸大小/形状),并将其转移到待切割成形的胶原膜上。接着,外科医生用特殊的锥子在软骨下骨板上制造微小的孔/骨折(微骨折手术)。血液和骨髓(含有骨髓基质干细胞)被释放形成含有软骨形成元素的血凝块。通过纤维蛋白胶(自体或市售)或缝合将正确尺寸的胶原膜贴附于微骨折区域。通过关节的屈曲,验证了胶原膜的稳定固定,最后关闭伤口。
First the cartilage defect is exposed and cleaned whereby all unstable degenerated cartilage, including the calcified cartilage layer, are carefully removed. An imprint of the defect is then taken using a sterile moldable material (e.g. aluminium foil) and transferred to the collagen membrane which is cut to shape. The surgeon then creates tiny holes/fractures in the subchondral bone plate (microfracturing) with a special awl. Blood and bone marrow (containing stem cells) are released forming a blood clot which contains cartilage forming elements. The correctly sized collagen membrane is added to the microfractured area either by fibrin glue (autologous or commercially available) or suturing. Through flexion of the joint, the stable positioning of the membrane is verified and the wound is closed.
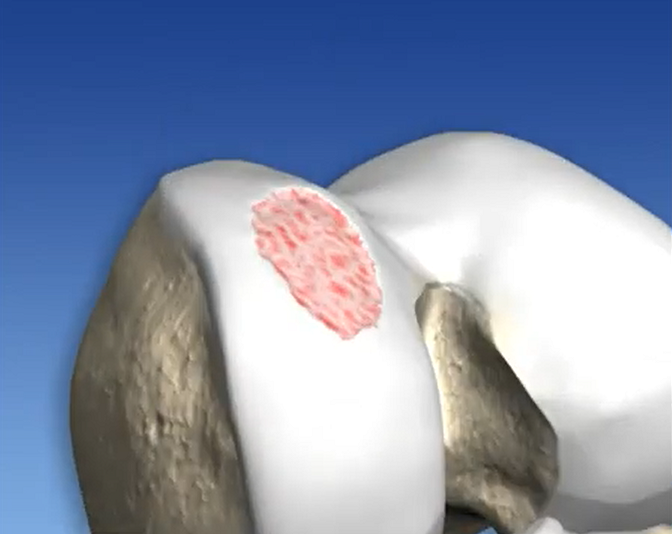
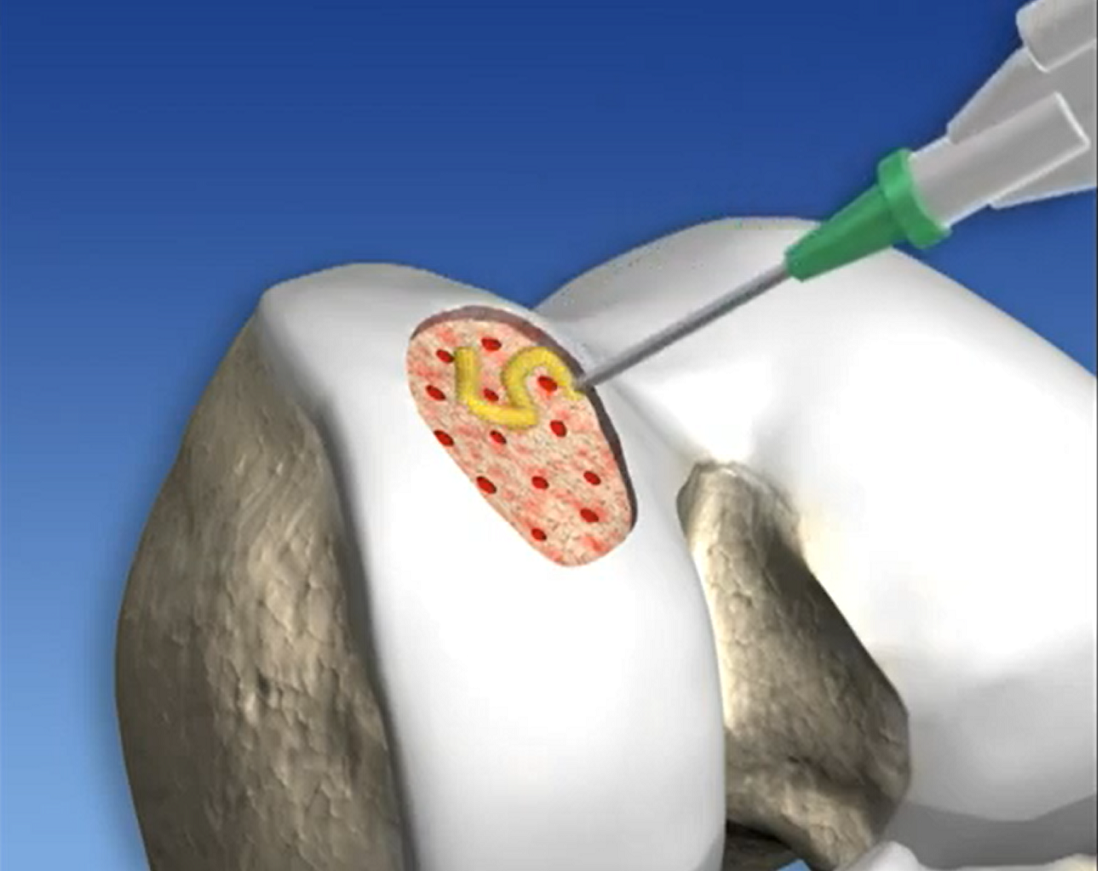
1.暴露并清理成形原软骨缺损,目的是小心去除所有不稳定的退化软骨,包括钙化的软骨下层
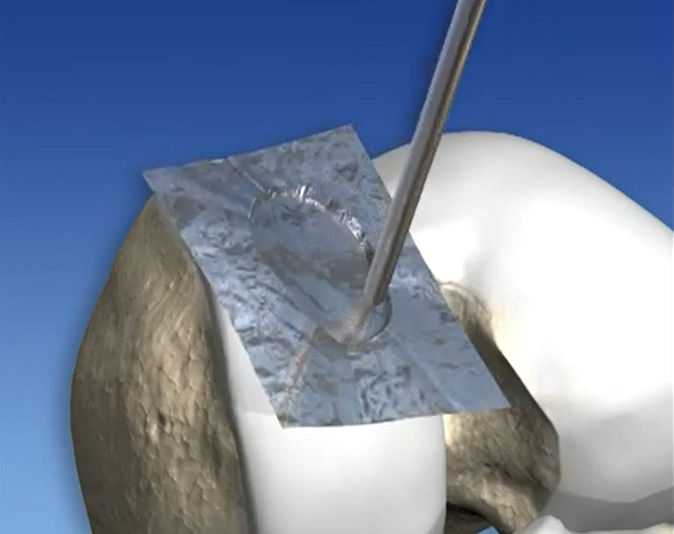

2. 使用无菌可压模材料(例如铝箔)获取缺陷的印记(尺寸大小/形状),并将其转移到待切割成形的胶原膜上

3. 外科医生用特殊的锥子在软骨下骨板上制造微小的孔/骨折(微骨折手术)
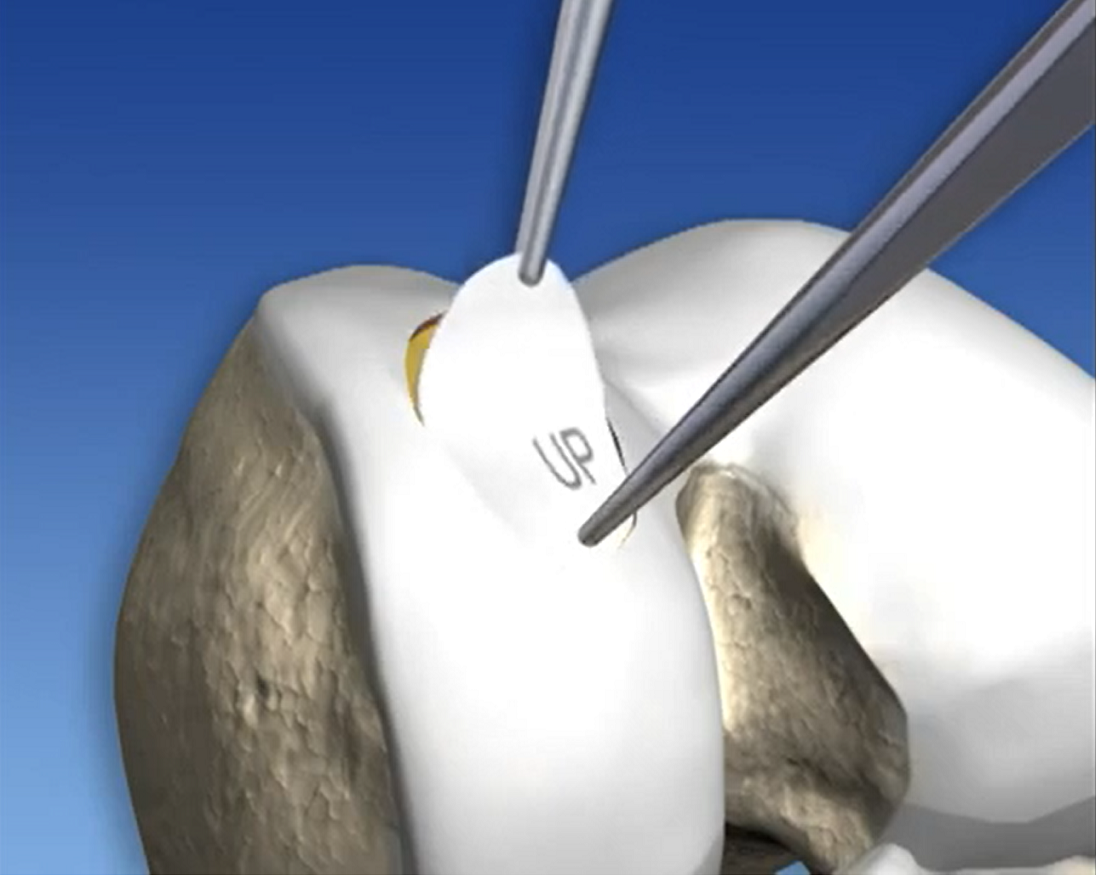
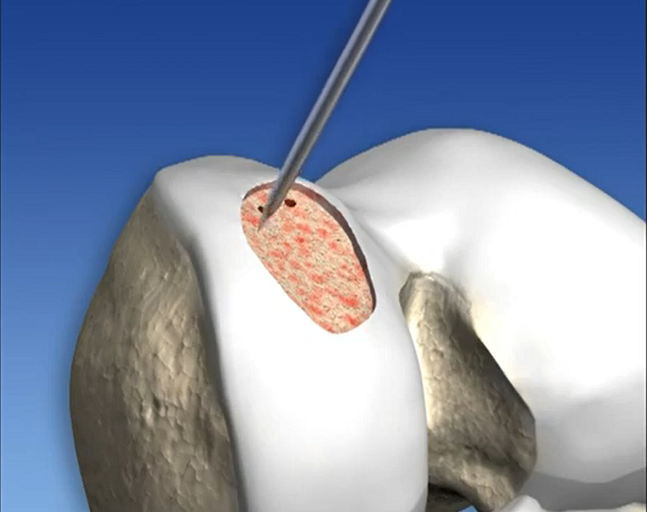
4. 通过纤维蛋白胶(自体或市售)或缝合将正确尺寸的胶原膜贴附于微骨折区域
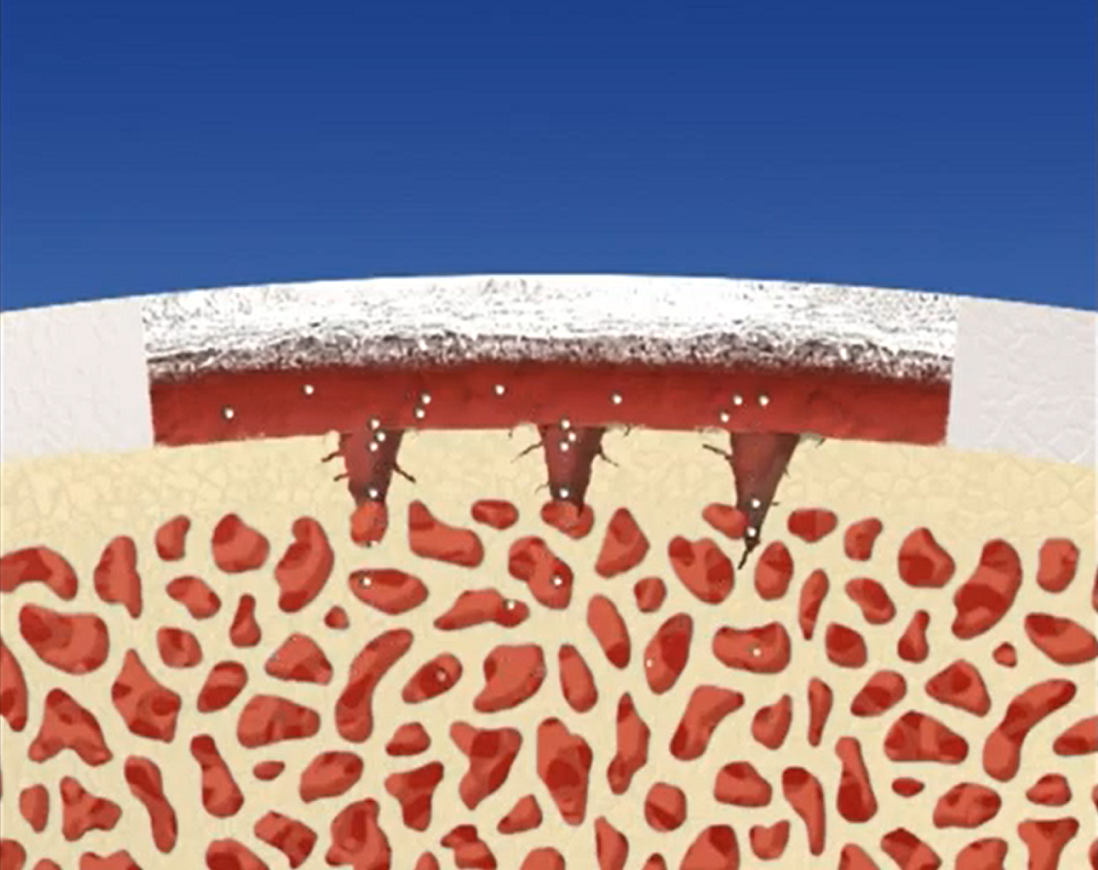

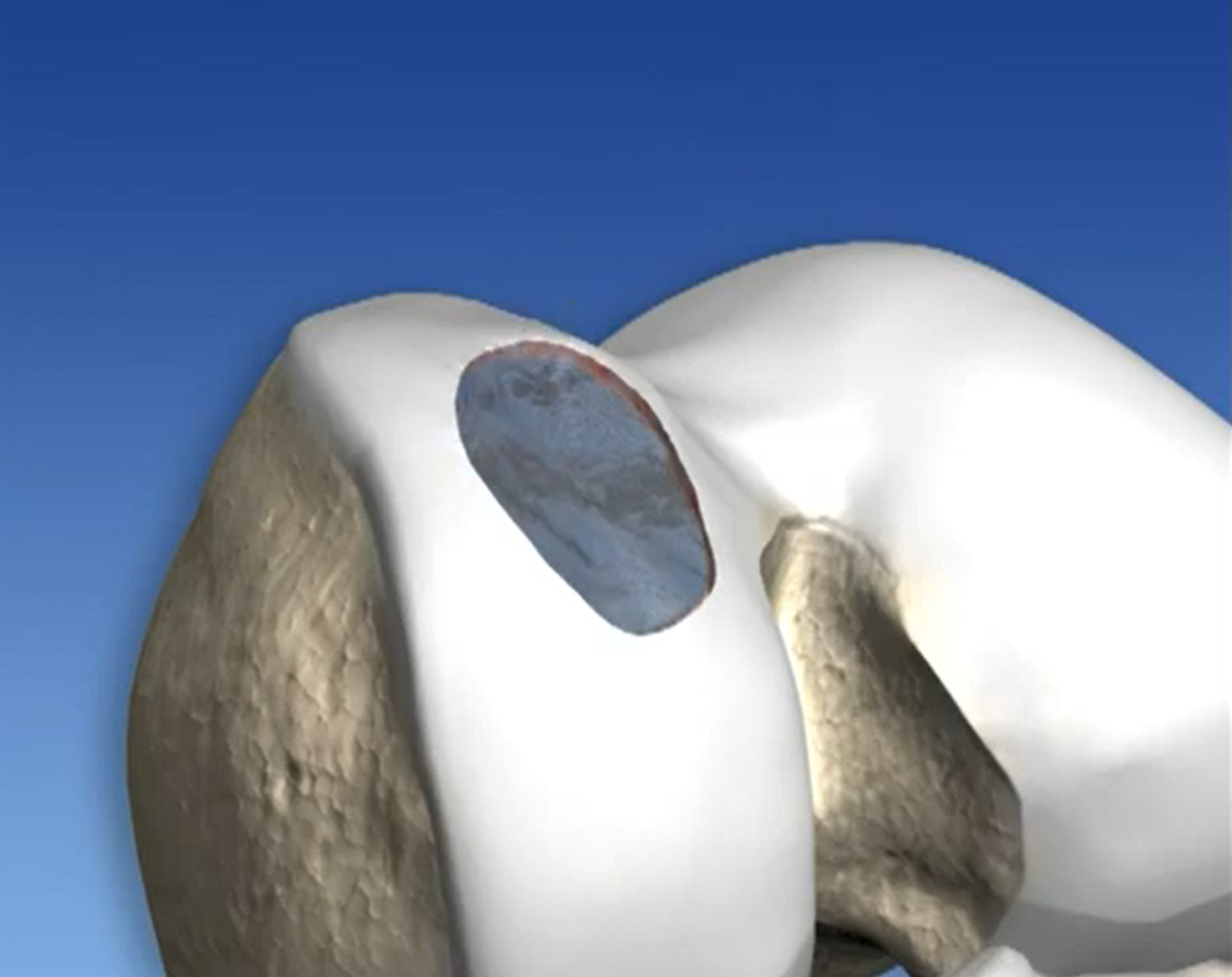
5. 血液和骨髓(含有骨髓基质干细胞)被释放形成含有软骨形成元素的血凝块
AMIC 手术满意结果的基本要求是遵守严格的治疗计划。存在指南和建议,尽管它们必须适应个体患者的需求。
An essential requirement for satisfying outcome of the AMIC surgery is the compliance to a strict physical therapy program. Guidelines and recommendations exist, though they have to be adapted to the individual patients needs.
AMIC手术由 Behrens 于 2003 年首次提出。它旨在将微骨折手术的使用范围扩大到 > 2.5 cm2 的较大软骨病变。 [5] 已经研究了AMIC在自体软骨细胞植入 (ACI) 中的临床效率,这是另一种用于较大软骨损伤的软骨修复技术。 [6][7][8]
History
The AMIC procedure was first proposed by Behrens in 2003. it aims to extend the use of microfracture surgery to larger cartilage lesions > 2.5 cm2.[5] Its clinical efficiency in autologous chondrocyte implantation (ACI), another cartilage repair technique for larger cartilage lesions, has been studied.[6][7][8]
一般来说,无论使用何种技术,已经确定了各种已知会影响软骨修复后结果的因素。其中包括个体和年龄、关节软骨缺损的大小和位置、手术技术和术后康复方案。 [9][10]后者被发现对于微骨折手术特别重要,对于 AMIC也是会如此 [11]
In general various factors have been identified known to influence the result after cartilage repair regardless of the technique used. Amongst them are the species and age of the individual, the size and localization of the articular cartilage defect, the surgical technique, and the postoperative rehabilitation protocol.[9][10] The latter has been found especially important for microfracture surgery and therefore for AMIC.[11]
微骨折手术的基本程序是 JR Steadman 在 80 年代末和 90 年代初开发的。这是一种临床报告疗效确切的针对较小面积的软骨病变的软骨修复的一线治疗选择。[12][13][14] AMIC 的发展旨在改善微骨折手术的一些不足之处,例如随着时间的推移修复软骨功能退化和软骨缺损面积较大的问题。 [15]
The basic procedure of Microfracture surgery was developed by JR Steadman in the late 80’s and early 90’s. It is a well documented cartilage repair technique and first line treatment option for small cartilage lesions.[12][13][14] AMIC evolved with the aim to improve some of the shortfalls of microfracture surgery as for instance variable repair cartilage volume and functional deterioration over time.[15]
References
Shaikh, N; Seah, MKT; Khan, WS (18 July 2017). “Systematic review on the use of autologous matrix-induced chondrogenesis for the repair of articular cartilage defects in patients“. World Journal of Orthopedics. 8 (7): 588–601. doi:10.5312/wjo.v8.i7.588. PMC 5534408. PMID 28808630.
“Deutsche Patent- und Markenamt (DPMA), registration # 30255356“. 2002-11-11. Retrieved 2013-01-25.
“World Intellectual Property Organization (WIPO), registration # 840373“. 2004-08-18. Retrieved 2013-01-25.
Piontek, Tomasz; Ciemniewska-Gorzela Kinga; Szulc Andrzej; Naczk Jakub; S?omczykowski Micha? (30 August 2011). “All-arthroscopic AMIC procedure for repair of cartilage defects of the knee“. Knee Surgery, Sports Traumatology, Arthroscopy. 20 (5): 922–925. doi:10.1007/s00167-011-1657-z. ISSN 0942-2056. PMC 3332359. PMID 21910000.
Behrens P., P. (2005). “Matrixgekoppelte Mikrofrakturierung“. Arthroskopie. 18 (3): 193–197. doi:10.1007/s00142-005-0316-0. S2CID 30000568.
Gomoll AH, Probst C, Farr J, Cole BJ, Minas T (November 2009). “Use of a type I/III bilayer collagen membrane decreases reoperation rates for symptomatic hypertrophy after autologous chondrocyte implantation“. Am J Sports Med. 37 Suppl 1: 20S–23S. doi:10.1177/0363546509348477. ISSN 0363-5465. PMID 19841142. S2CID 206524323.
Steinwachs M, Kreuz PC (April 2007). “Autologous chondrocyte implantation in chondral defects of the knee with a type I/III collagen membrane: A prospective study with a 3-year follow-up“. Arthroscopy. 23 (4): 381–387. doi:10.1016/j.arthro.2006.12.003. ISSN 1526-3231. PMID 17418330.
Gooding CR, Bartlett W, Bentley G, Skinner JA, Carrington R, Flanagan A (Jun 2006). “A prospective, randomised study comparing two techniques of autologous chondrocyte implantation for osteochondral defects in the knee: Periosteum covered versus type I/III collagen covered“. Knee. 13 (3): 203–10. doi:10.1016/j.knee.2006.02.011. ISSN 0968-0160. PMID 16644224.
Alford JW, Cole BJ (Mar 2005). “Cartilage restoration, part 2: techniques, outcomes, and future directions“. Am J Sports Med. 33 (3): 443–460. doi:10.1177/0363546505274578. ISSN 0363-5465. PMID 15716263. S2CID 11361026.
Steinwachs MR, Guggi T, Kreuz PC (Apr 2008). “Marrow stimulation techniques“. Injury. 39 Suppl 1: S26–31. doi:10.1016/j.injury.2008.01.042. ISSN 0020-1383. PMID 18313469.
Hurst JM, Steadman JR, O‘Brien L, Rodkey WG, Briggs KK (Apr 2010). “Rehabilitation following microfracture for chondral injury in the knee“. Clin Sports Med. 29 (2): 257–65, viii. doi:10.1016/j.csm.2009.12.009. ISSN 1556-228X. PMID 20226318.
Steadman JR, Rodkey WG, Singleton SB, Briggs KK (October 1997). “Microfracture technique for full-thickness chondral defects: Technique and clinical results“. Oper Tech Orthop. 7 (4): 300–304. doi:10.1016/S1048-6666(97)80033-X.
Steadman JR, Rodkey WG, Rodrigo JJ (Oct 2001). “Microfracture: surgical technique and rehabilitation to treat chondral defects“. Clin Orthop Relat Res. 391 (391 Suppl): S362–9. doi:10.1097/00003086-200110001-00033. ISSN 0009-921X. PMID 11603719.
Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG (May–Jun 2003). “Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up“. Arthroscopy. 19 (5): 477–84. doi:10.1053/jars.2003.50112. ISSN 1526-3231. PMID 12724676.
Mithoefer K, McAdams T, Williams RJ, Kreuz PC, Mandelbaum BR (Oct 2009). “Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis“. Am J Sports Med. 37 (10): 2053–63. doi:10.1177/0363546508328414. ISSN 1552-3365. PMID 19251676. S2CID 206523609.
图片与文字来源Wikipedia, google image & YouTube.
本文是陶可版权所有,未经授权请勿转载。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论