
膝关节软骨损伤Recht MRI分级_MR技术分析膝关节软骨病变(1993)
膝关节软骨损伤Recht MRI分级_MR技术分析膝关节软骨病变(1993)Abnormalities of articular cartilage in the knee: analysis of available MR techniques
Recht M P, Kramer J, Marcelis S, Pathria M N, Trudell D, Haghighi P, Sartoris D J, Resnick D. Abnormalities of articular cartilage in the knee: analysis of available MR techniques[J]. Radiology, 1993,187(2): 473-478.
转载文章的原链接1:
https://pubmed.ncbi.nlm.nih.gov/8475293/
转载文章的原链接2:
https://pubs.rsna.org/doi/10.1148/radiology.187.2.8475293?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
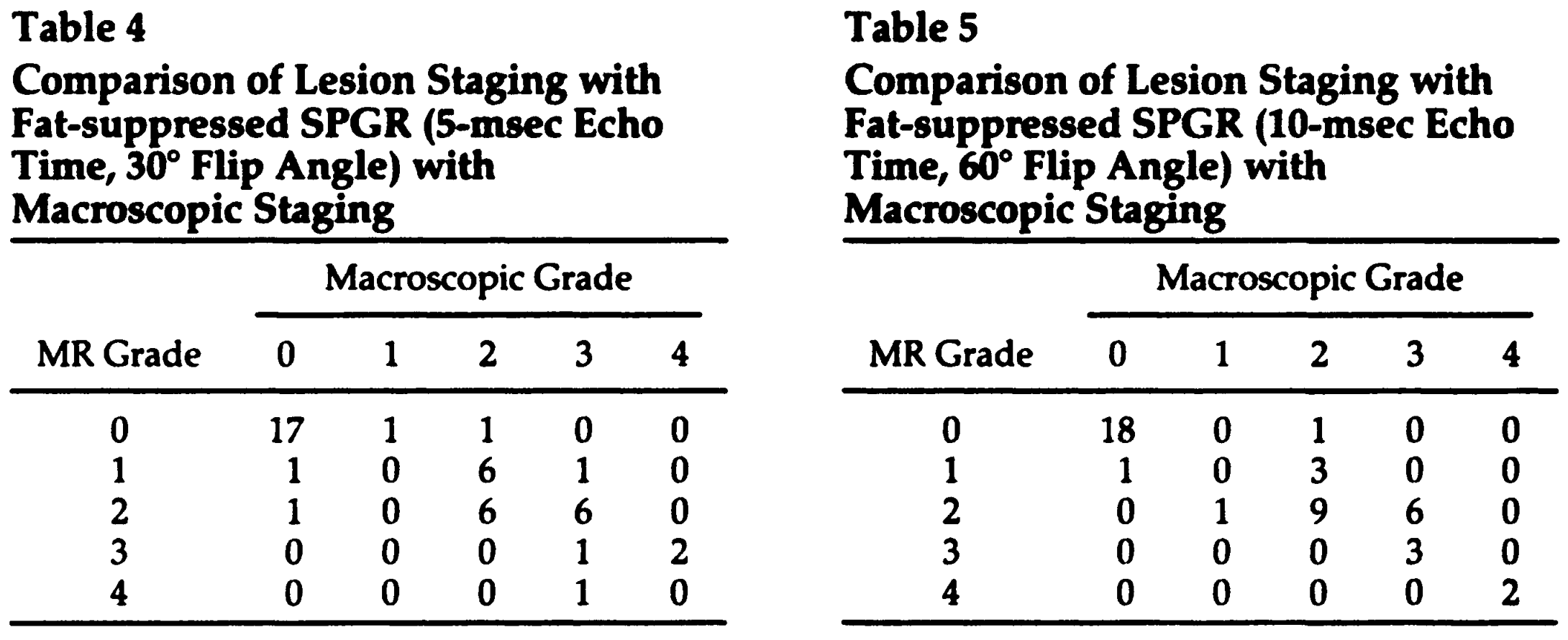
软骨损伤Recht MRI分级
0 级:正常关节软骨,软骨弥漫性均匀变薄但表面光滑,仍认为是正常关节软骨;
Ⅰ级:软骨分层结构消失,软骨内出现局限性低信号区,软骨表面光滑;
Ⅱ级:软骨表面轮廓轻至中度不规则,软骨缺损深度未及全层厚度的50%;
Ⅲ级:软骨表面轮廓重度不规则,软骨缺损深达全层厚度的50%以上,但未完全剥脱;
Ⅳ级:软骨全层剥脱、缺损,软骨下骨暴露伴或不伴软骨下骨质信号改变。
Rubenstein和Recht等通过研究发现SE序列和3D FS SPGR序列可以将正常的关节软骨显现为三层,表层相是切线层、过渡层和放射层的上部,中间层是放射层的大部,深层是放射层的下部。结合Recht对软骨损伤的分级,软骨退变在I~II级时,损伤的为软骨的切线层及过渡层,即为软骨的轻度损伤,如累及放射层以下则为软骨的中、重度损伤。
Abstract
In an attempt to improve the detection of chondral abnormalities with magnetic resonance imaging, a fat-suppressed three-dimensional gradient-recalled acquisition in the steady state (GRASS) and spoiled GRASS (SPGR) sequence was optimized by study of five cadaveric knee specimens. Results with this optimized sequence then were compared with results with three spin-echo (T1-, proton-density-, and T2-weighted) and two three-dimensional gradient-recalled echo sequences (GRASS and non-fat-suppressed SPGR) in the assessment of naturally occurring abnormalities of the patellofemoral compartment in 10 cadaveric knees. Results with the optimized fat-suppressed SPGR sequence were significantly better (P < .02) than results with the other five sequences and had a sensitivity of 96%, a specificity of 95%, and an accuracy of 95%. In addition, normal cartilage consistently appeared as a trilaminar structure with the fat-suppressed SPGR sequence, a feature that appeared to help in identification of chondral lesions.
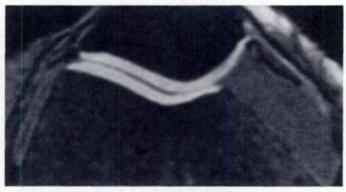
Figure 1. Fat-suppressed SPGR image (52/ 10, with flip angle of 60°) of normal cartilage. Cartilage appears as a structure with high signal intensity compared with both fluid and bone marrow. Note the trilaminar appearance of the normal cartilage, which is best appreciated on the lateral patellar facet and lateral femur. Specimen was from a 70-year-old woman.
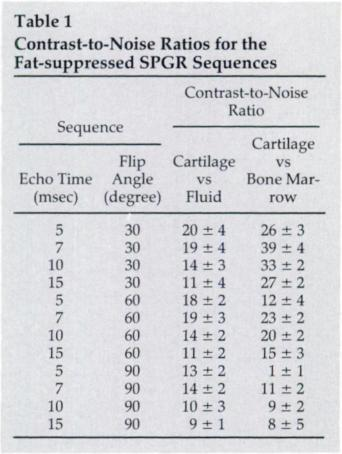
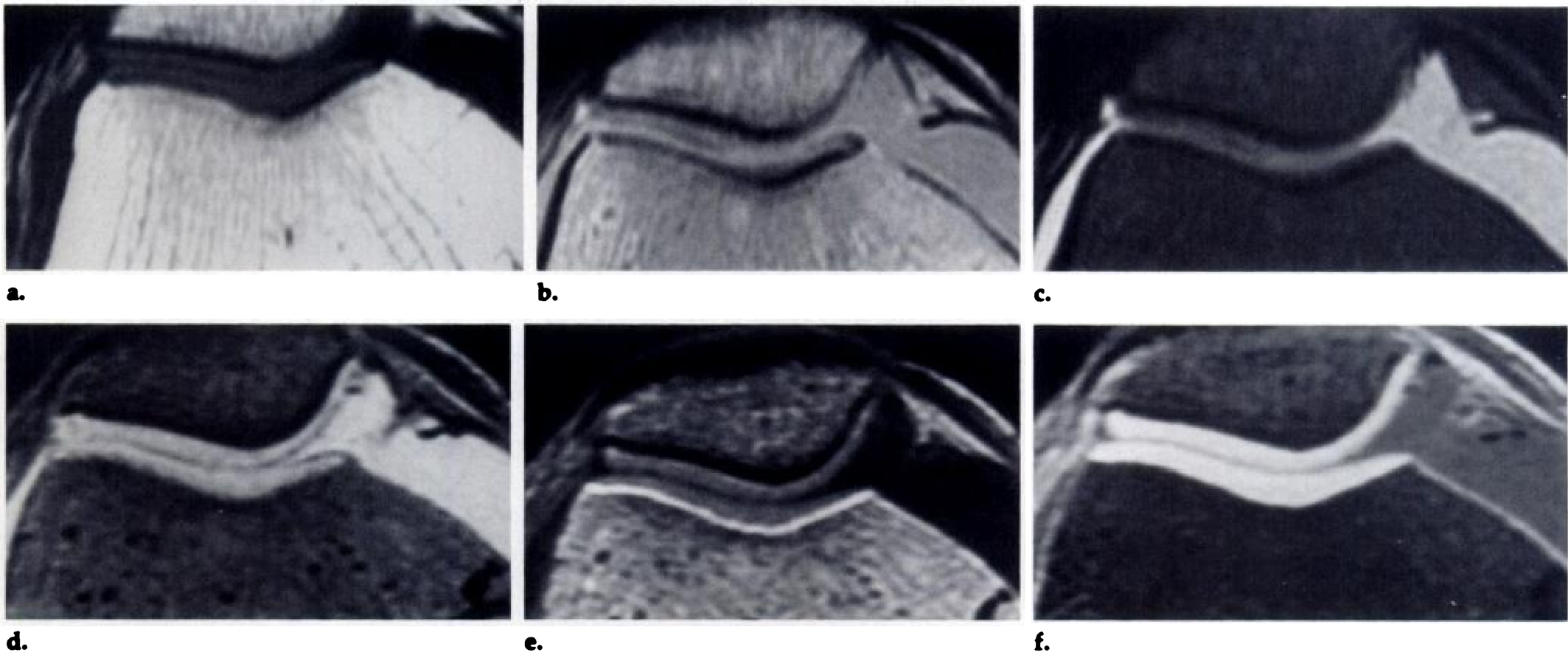
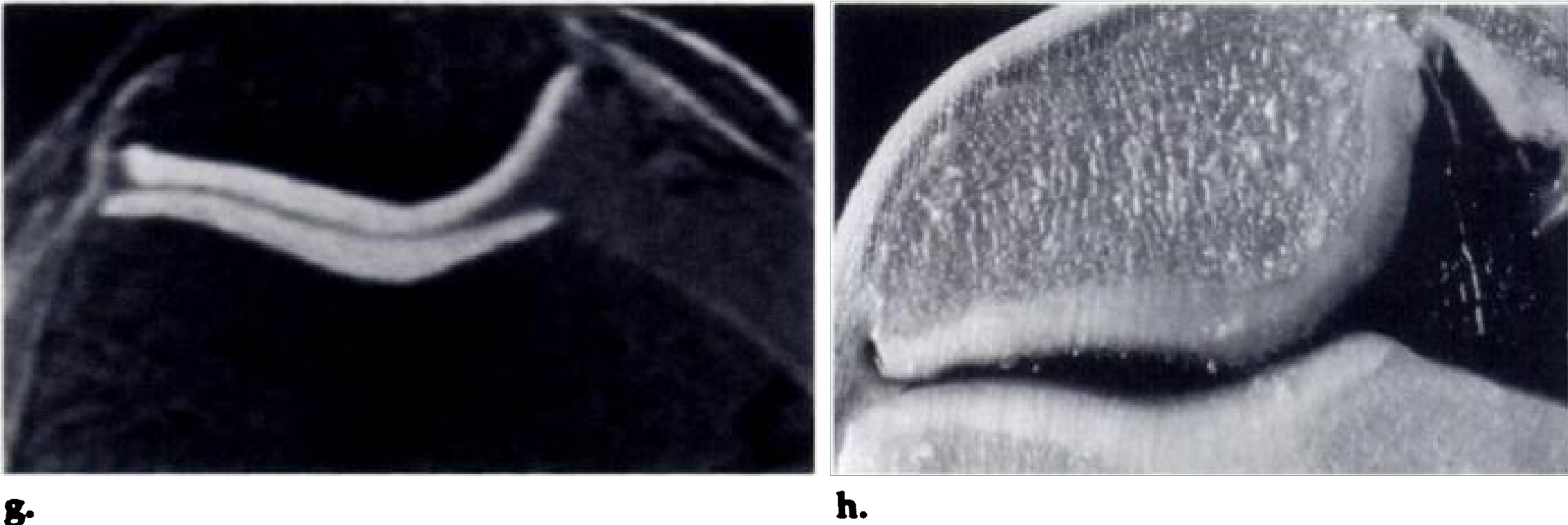
Figure 2. Surface fibrillation of the medial patellar facet in a specimen from an 83-year-old woman.
(a) Ti-weighted (500/14) image.
(b) Proton-density-weighted (2,000/20) image.
(c) T2-weighted (2,000/70) image.
(d) GRASS (40/10, with flip angle of 30°)image.
(e) SPGR (40/5, with flip angle of 30°) image.
(f) (0 Fat-suppressed SPGR (52/5, with flip angle of 30°)image.
(g) Fat-suppressed SPGR (52/10, with a flip angle of 60°)image.
(h) Corresponding anatomic section. Note the fine surface fibrillation of the medial patellar facet, corresponding to a grade 2 lesion. This is difficult to appreciate on the spin-echo images and is best demonstrated on the fat-suppressed SPGR images.
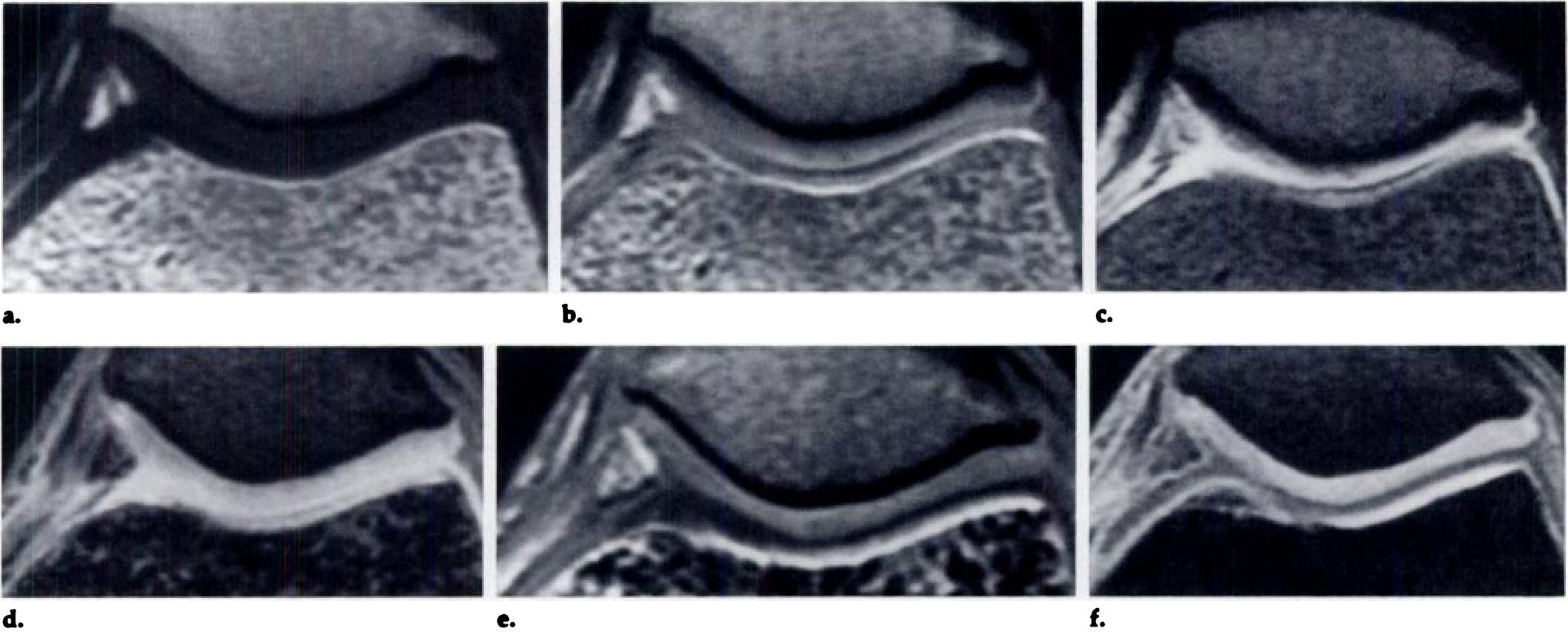
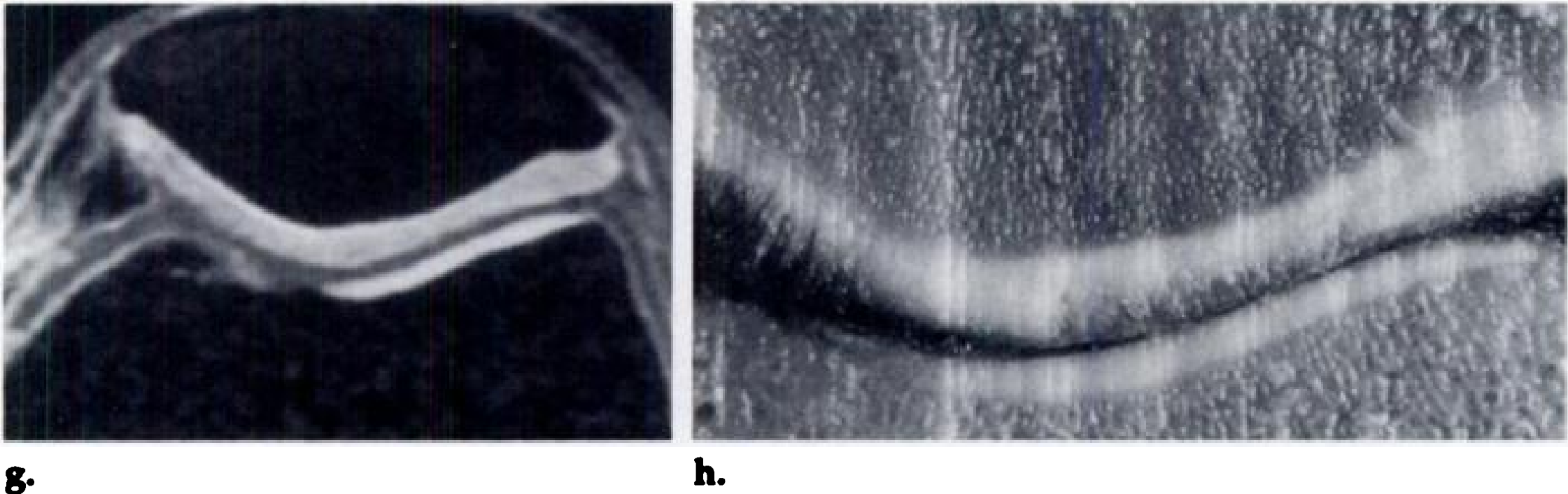
Figure 3. Grade 2 lesion of the lateral patellar facet and grade 3 lesion of the medial patellar facet in a specimen from an 80-year-old man.
(a) TI-weighted (500/14) image.
(b) Proton-density-weighted (2,000/20) image.
(c) T2-weighted (2,000/70) image.
(d) GRASS (40/10, with a flip angle of30°)image.
(e)SPGR (40/5, with a flip angle of 30°)image.
(f) Fat-suppressed SPGR (52/5, with a flip angle of 30°)image.
(g) Fat-suppressed SPGR (52/10, with a flip angle of 60°)image.
(h) Corresponding anatomic section. Note the superior depiction of the lesions on the fat-suppressed SPGR images and their excellent correlation with the anatomic specimen. The surface layer of cartilage with high signal intensity on the fat-suppressed SPGR images is interrupted in the region of the cartilage lesions. The absence of cartilage on the medial femoral condyle is secondary to the plane of sectioning and is not a true cartilage lesion.
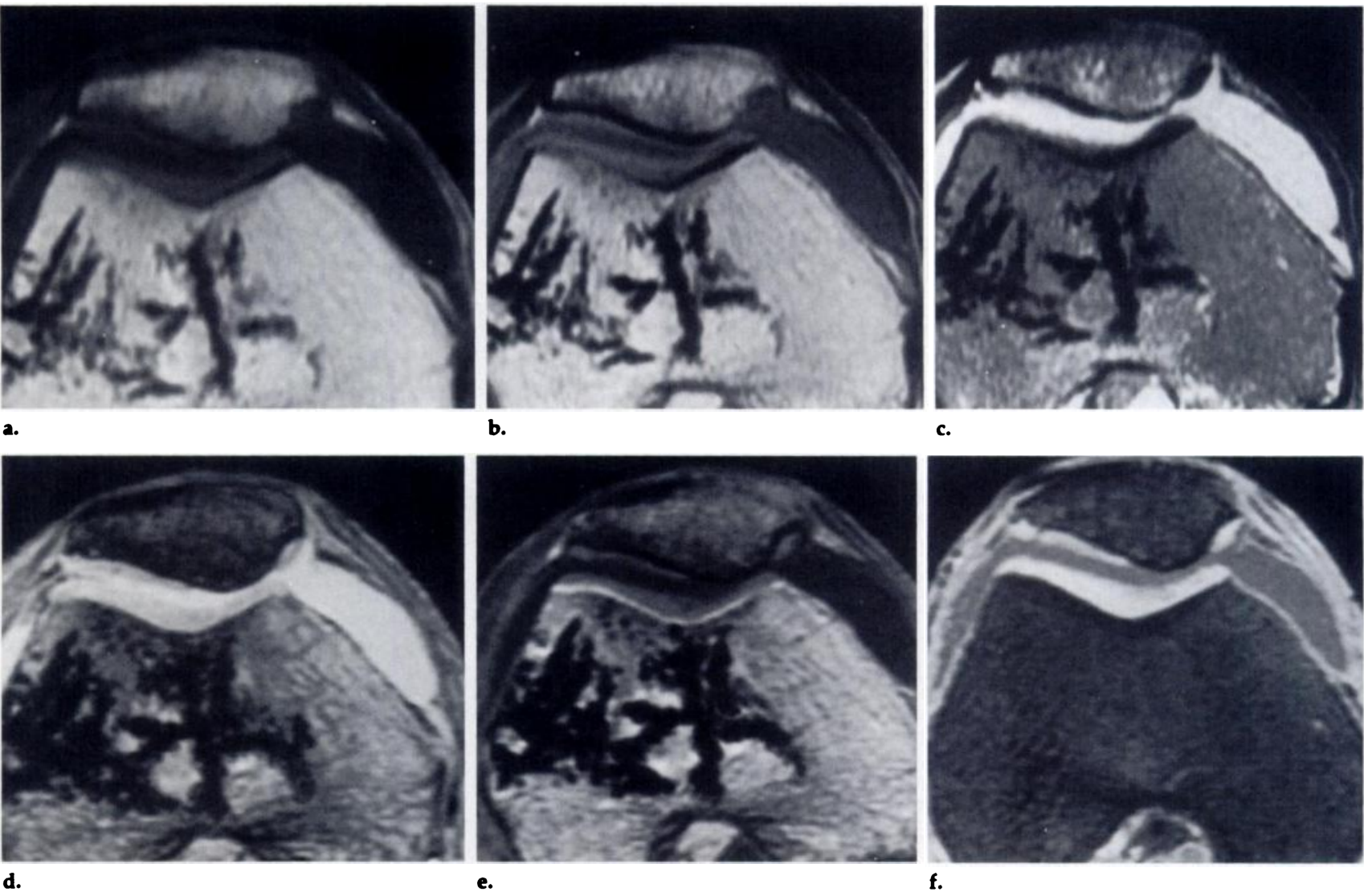
Figure 4. Grade 4 patellar lesion and grade 3 femoral lesion in a specimen from an 84-year-old woman.
(a) Ti-weighted (500/i4) image.
(b) Proton-density-weighted (2,000/ 20) image.
(c) T2-weighted (2,000/70) image.
(d) GRASS (40/10, with a flip angle of 30°) image.
(e) SPGR (40/5, with a flip angle of 30°)image.
(f) Fat-suppressed SPGR (52/5, with a flip angle of 30°) image.
(g) Fat-suppressed SPGR (52/10, with a flip angle of 60°) image.
(h) Corresponding anatomic section. The patellar lesion is well visualized with all sequences, but the femoral lesion is best visualized on the fat-suppressed SPGR images, especially the sequence with echo time of 10 msec and a flip angle of 60°
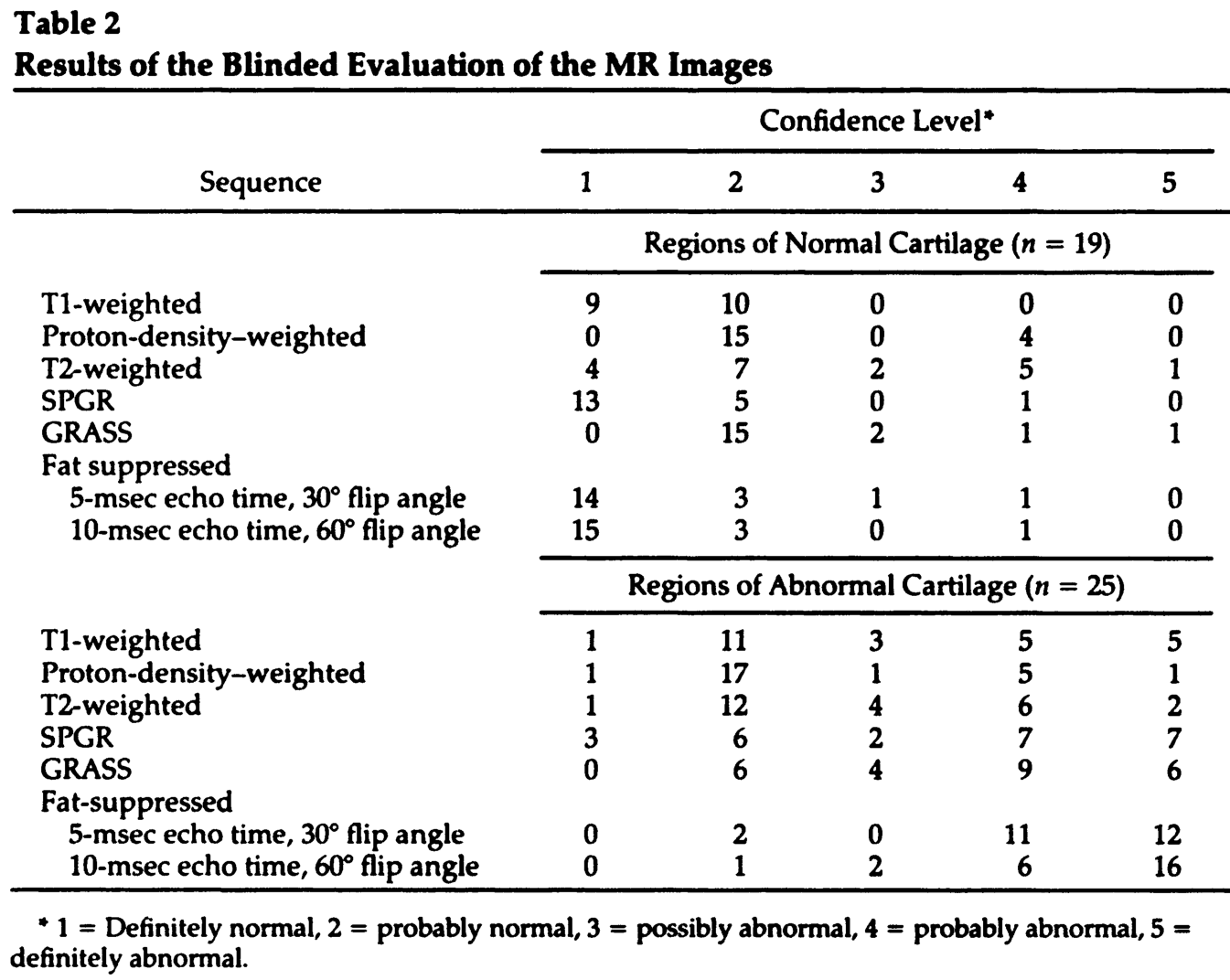
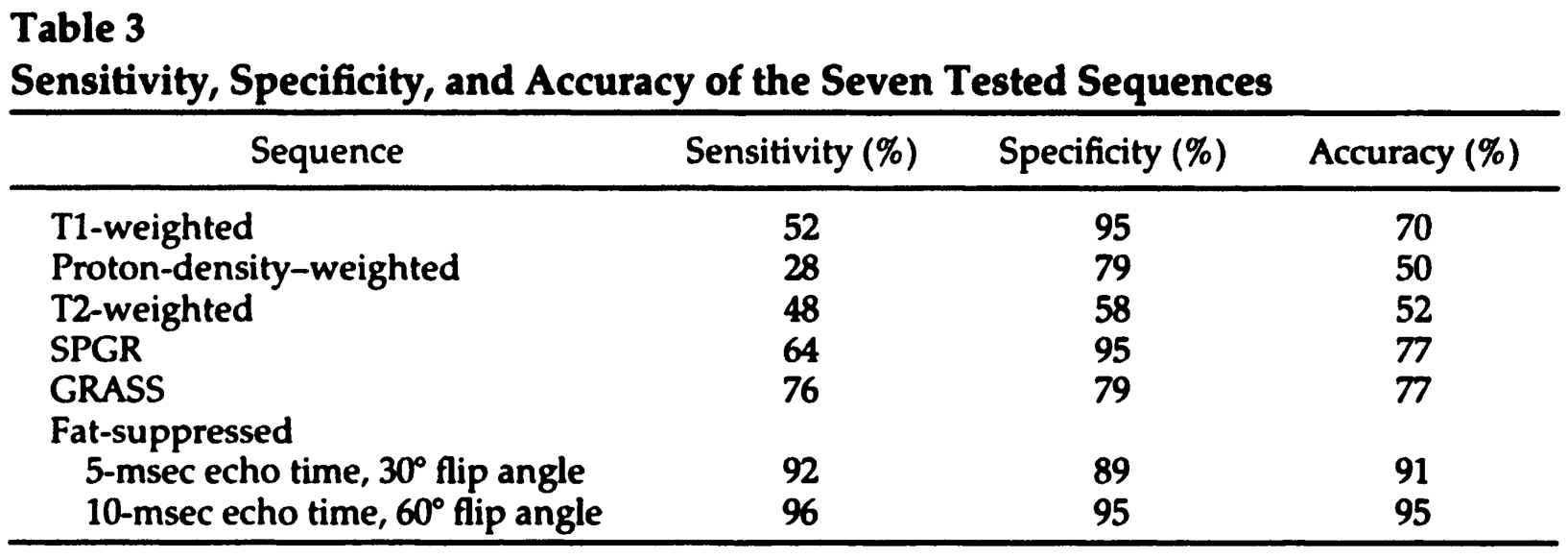
In summary, a fat-suppressed SPGR sequence was optimized for the detection of articular cartilage abnormalities and resulted in acquisition of significantly better findings in the assessment of cartilage lesions than was possible with a number of spin-echo and GRE sequences. In addition, cartilage was routinely demonstrated to be trilaminar in appearance with the fat-suppressed SPGR sequences. Further clinical and histologic studies are warranted with the fat-suppressed SPGR sequence to confirm its clinical usefulness.

本文为转载文章,如有侵权请联系作者删除。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论