 三甲
三甲
髋臼发育不良:美国临床运动医学杂志2021年研究进展
髋臼发育不良:美国临床运动医学杂志2021年研究进展
作者:Joshua D Harris, Brian D Lewis, Kwan J Park
作者单位: The Houston Methodist Hip Preservation Program, Houston Methodist Orthopedics and Sports Medicine, 6445 Main Street, Suite 2500, Houston, TX 77030, USA; Houston Methodist Academic Institute; Houston Methodist Orthopedics & Sports Medicine, Houston, TX, USA; Weill Cornell Medical College, New York, NY, USA; Texas A&M University, College Station, TX, USA. Electronic address: joshuaharrismd@gmail.com.
译者:陶可(北京大学人民医院骨关节科)
摘要
髋臼发育不良代表与髋部疼痛、不稳定和骨关节炎相关的结构病理形态。广泛的不典型增生在解剖学上是指基于3维体积和表面积的覆盖不足,并根据覆盖不足的程度和位置进行分类。临界髋臼发育不良的定义各不相同,并导致治疗方式的不统一。对于有症状的髋臼发育不良,治疗采用髋臼周围截骨术。同步或分期髋关节镜检查对于解决关节内病理学具有显着优势。在非髋关节骨关节炎个体中,有证据表明PAO可以改变髋臼发育不良的自然病史,并降低髋关节骨关节炎和全髋关节置换术的风险。
诊所诊治要点
①髋臼发育不良是一种复杂的多平面结构病理形态,与髋部疼痛、不稳定和髋关节骨关节炎紧密相关。
②髋臼发育不良的自然病史导致继发于高度复杂的基于3-维度体积和表面积的覆盖范围不足软骨损伤。
③髋臼发育不良可以通过其位置来表征定位:前部、后部或外侧部(或整体)。
④髋臼发育不良的评估需要X线片和MRI、CT扫描,以衡量正常的覆盖范围和角度。
⑤单纯髋关节镜检查不应用于治疗中度或严重髋臼发育不良所致的髋关节解剖结构不稳定。
⑥在正确选择的具有过渡性髋臼覆盖或临界髋臼发育不良的患者中,短期和中期的随访可以取得良好的效果。
PAO和髋关节镜检查可以同时或分阶段一起使用,以准确地纠正髋臼发育不良和FAI髋关节撞击综合征。
⑦在非髋关节骨关节炎个体中,PAO改变了髋臼发育异常的自然病史并降低了以下风险:髋关节骨关节炎和随后的THA全髋关节置换术。
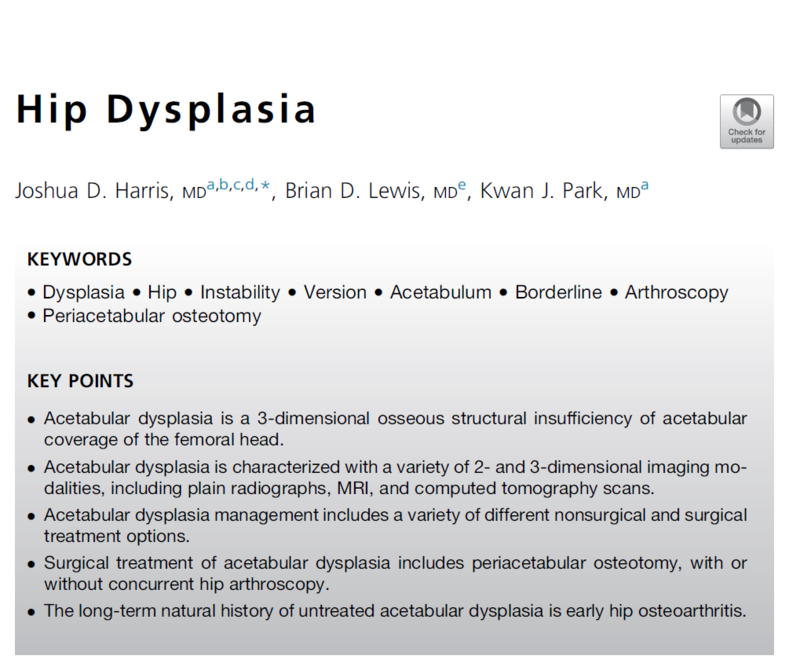
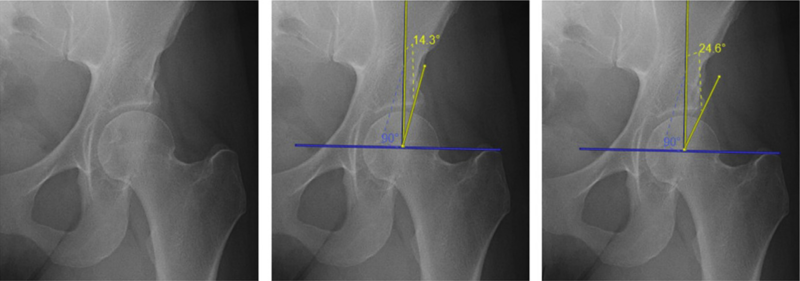
Fig. 1. Weight-bearing AP pelvis plain radiograph with focus on left hip in 17-year-old girl (left) showing an LCEA of 14.3° measured to the lateral sourcil (middle) and 24.6° measured to the lateral acetabular bone (right).
图1. 17岁女孩的负重前后位(AP)骨盆X线片,左髋(左);LCEA测量值为14.3°(中);测量到髋臼骨性外侧边缘为24.6°(右)。
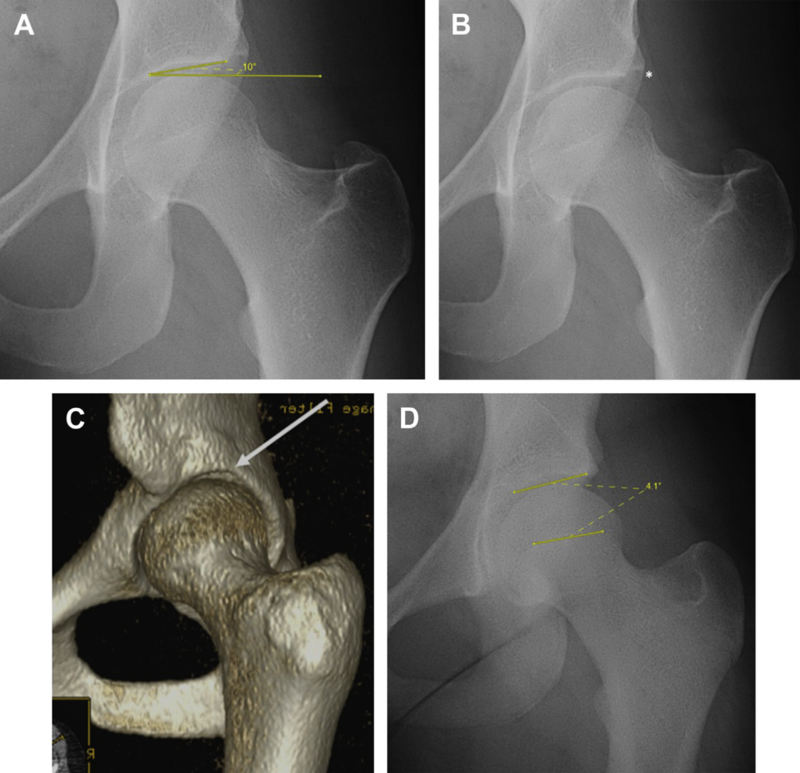
Fig. 2. (A) Weight-bearing AP pelvis plain radiograph with focus on left hip in 19-year-old woman showing a Tonnis angle of 10°. (B) An upsloping lateral sourcil (asterisk). (C) Upsloping lateral sourcil in the same patient visualized on 3-dimensional computed tomography scan; and (D) a FEAR Index of 4.1°.
图2. (A) 19岁女性的负重前后位(AP)骨盆X线片,重点关注左髋,Tonnis角为10°。(B)向上倾斜的眉弓(星号)。(C)在3维计算机断层扫描中显示同一患者的向上倾斜的眉弓;(D) FEAR指数为4.1°。femoroepiphyseal acetabular roof:股骨骨骺髋臼顶
The FEAR index has value in the evaluation of hip instability (femoral head migration on conventional plain radiographs or head recentering on an AP abduction view) in patients with transitional acetabular coverage.
FEAR指数对于评估具有过渡性髋臼覆盖的患者的髋关节不稳定性(传统X线片上的股骨头移位或AP外展视图上的股骨头复位)具有价值。
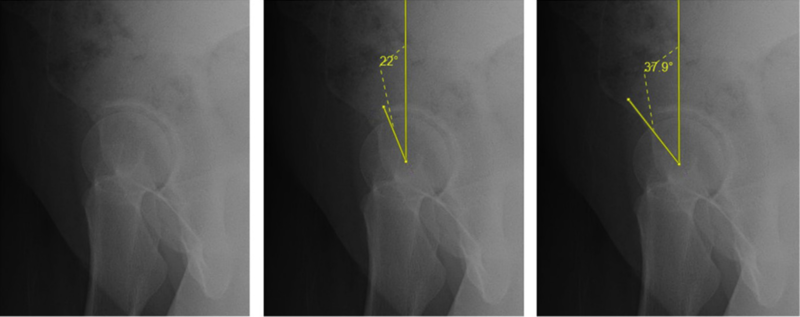
Fig. 3. False profile plain radiograph of right hip in 21-year-old woman (left) showing an ACEA of 22° measured to the anterior sourcil (middle image) and 37.9° measured to the anterior acetabular bone (right).
图3. 21岁女性右髋部的假斜位X线片(左);ACEA测量到髋臼关节面前缘的角度为22°(中);测量到髋臼前缘骨质的角度为37.9°(右)。

Fig. 4. Weight-bearing AP pelvis plain radiograph with focus on right hip in 24-year-old man showing the measurements needed to calculate the AWI and the PWI. A best-fitting perfect circle is drawn around the femoral head. A line is drawn connecting the femoral neck center intersecting with the head center. AWI = AW/r; PWI = PW/r.
图4. 24岁男性的负重前后位(AP)骨盆X线片,重点关注右髋,显示计算AWI和PWI所需的测量值。在股骨头周围绘制一个最合适的完美圆。绘制一条连接股骨颈中心与股骨头中心相交的线。AWI = AW/r; PWI = PW/r。
PWI: the posterior wall index; AWI: anterior wall index.
PWI:后壁指数;AWI:前壁指数。
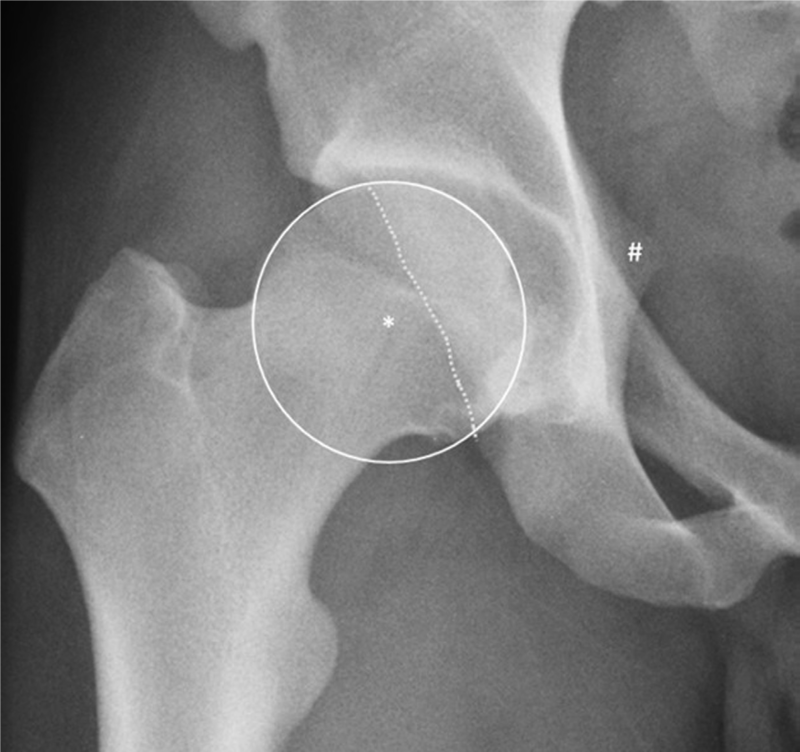
Fig. 5. Weight-bearing AP pelvis plain radiograph with focus on right hip in 31-year-old man demonstrating a positive posterior wall sign (*) and positive ischial spine sign (#).
图5. 31岁男性的负重前后位(AP)骨盆X线片,重点关注右髋,后壁征(*)和坐骨棘征(#)阳性。
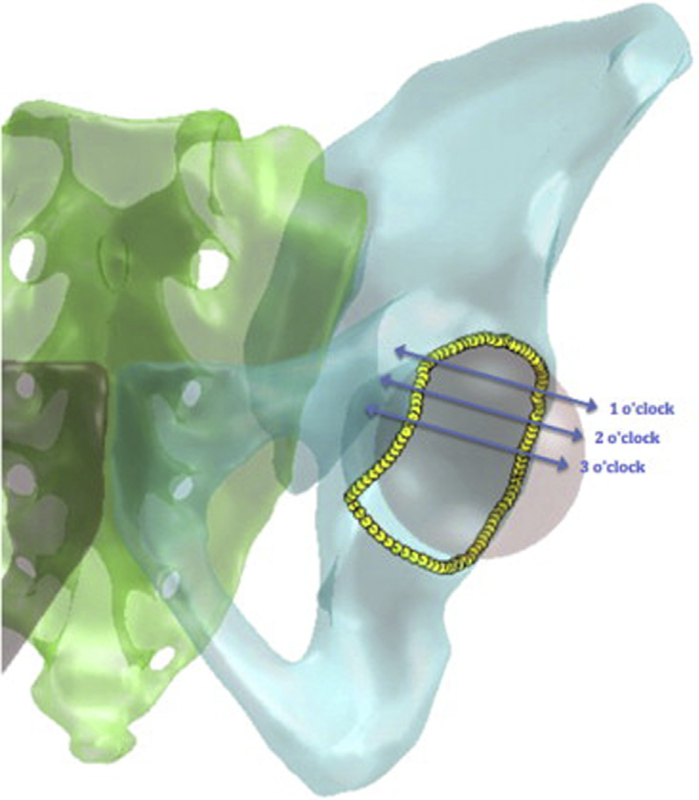
Fig. 6. Clock-face positions of version measurements. This 3-dimensional model depicts the 3 different locations we used to measure focal acetabular version (1, 2, and 3 o’clock). (From Tannenbaum EP, Zhang P, Maratt JD, et al. A Computed Tomography Study of Gender Differences in Acetabular Version and Morphology: Implications for Femoroacetabular Impingement. Arthroscopy 2015;31:1247–54; with permission.)
图6. 髋臼测量的钟面位置。这个3维模型描绘了我们用来测量髋臼局部区域的3个不同位置视图(1点、2点和3点钟方向)。
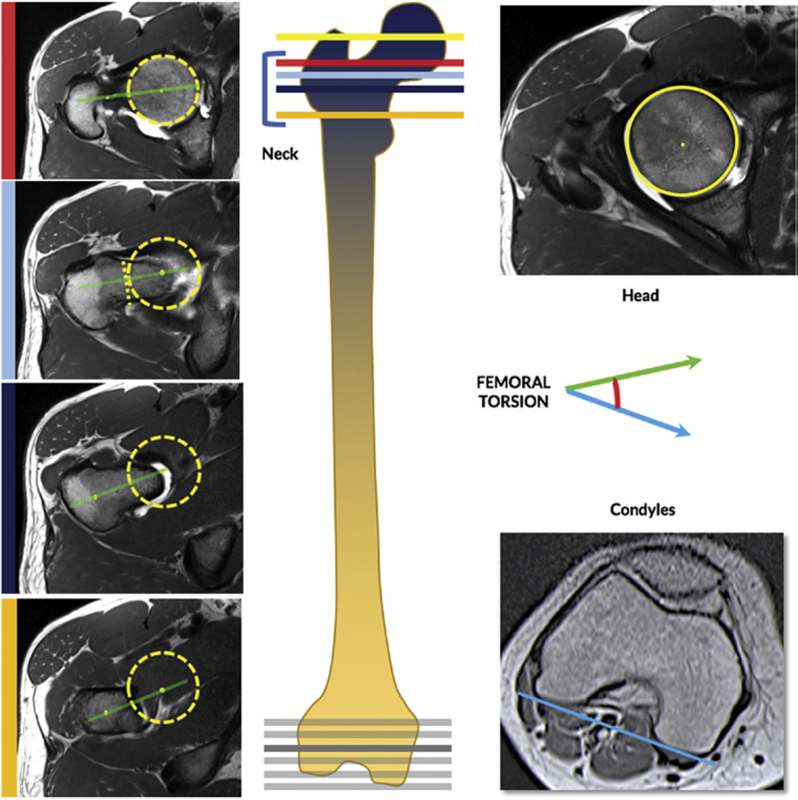
Fig. 7. Assessment of femoral torsion on cross-sectional imaging. On consecutive strict axial images over the proximal femur, determine the femoral head center (FHC) (yellow circle and yellow line). Defining the femoral neck axis (green line) can be done by several methods. Lee method (red bar): A line is drawn on the first image on which the FHC can be connected with the most cephalic junction of the greater trochanter and the femoral neck; Reikeras method (light blue bar): A line connecting the FHC with the femoral neck center is drawn on an image where the anterior and posterior cortices run parallel to each other; Jarret method (not shown): A line is drawn on a single image that runs from the FHC trough the center of the femoral neck; Tomczak method (dark blue bar): The FHC is connected with the center of the greater trochanter at the base of the femoral neck; and Murphy method (orange bar): The FHC is connected with the center of the base of the femoral neck directly superior to the lesser trochanter. Then, over the distal femur, draw a tangent to the posterior aspect of the femoral condyles (blue line; choosing the slice where the condyles are more prominent). The angle between both lines represents the femoral torsion. Although some of these reference points are located on different adjacent slices, modern workstations should allow drawing and modifying a line across multiple images in 1 series or, alternatively, different slices can be superimposed on a single image with the help of postprocessing software. (From Mascarenhas VV, Ayeni OR, Egund N, et al. Imaging Methodology for Hip Preservation: Techniques, Parameters, and Thresholds. Semin Musculoskelet Radiol 2019;23:197-226; with permission.)
图7. 横截面成像评估股骨扭转角度。在股骨近端的连续严格轴向图像上,确定股骨头中心(FHC)(黄色圆圈和黄线)。可以通过多种方法来定义股骨颈轴(绿线)。Lee法(红条):在第一张图像上画一条线,将FHC与大转子和股骨颈的最头连接处连接起来;Reikeras方法(浅蓝色条):在图像上绘制连接FHC与股骨颈中心的线,其中前皮质和后皮质彼此平行; Jarret方法(未显示):在单个图像上绘制一条从FHC穿过股骨颈中心的线;Tomczak法(深蓝色条):FHC与股骨颈基部大转子中心相连;墨菲法(橙色条):FHC与小转子正上方的股骨颈基底部中心相连。然后,在股骨远端上,绘制股骨髁后部的切线(蓝线;选择髁更突出的切片)。两条线之间的角度代表股骨扭转角度。尽管其中一些参考点位于不同的相邻切片上,但现代工作站应该允许在1系列中的多个图像上绘制和修改一条线,或者,可以借助后处理软件将不同的切片叠加在单个图像上。
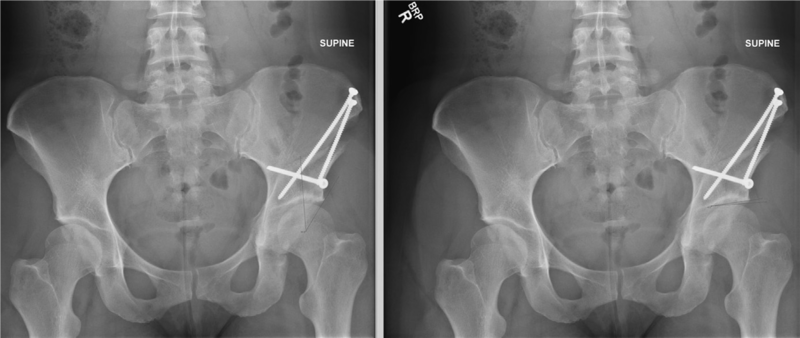
Fig. 8. Postoperative AP pelvis plain radiograph following PAO (Periacetabular osteotomy) of left hip in 20-year-old woman with an LCEA of 34° (left) and a Tonnis angle of 3° (right).
图8. 20岁女性左髋PAO(髋臼周围截骨术)术后前后位(AP)骨盆X线片,LCEA为34°(左),Tonnis角为3°(右)。
Hip Dysplasia
Abstract
Acetabular dysplasia represents a structural pathomorphology associated with hip pain, instability, and osteoarthritis. The wide spectrum of dysplasia anatomically refers to a 3-dimensional volumetric- and surface area-based insufficiency in coverage and is classified based on the magnitude and location of undercoverage. Borderline dysplasia has been variably defined and leads to management challenges. In symptomatic dysplasia, treatment addresses coverage with periacetabular osteotomy. Concomitant simultaneous or staged hip arthroscopy has significant advantages to address intra-articular pathology. In nonarthritic individuals, there is evidence PAO alters the natural history of dysplasia and decreases the risk of hip arthritis and total hip arthroplasty.
CLINICS CARE POINTS
Acetabular dysplasia is a complex multiplanar structural pathomorphology associated with hip pain, instability, and osteoarthritis.
The natural history of dysplasia leads to chondral injury secondary to the highly complex 3- dimensional volumetric- and surface area-based insufficiency in coverage.
Dysplasia can be characterized by its location: anterior, posterior, or lateral (or global).
Evaluation of dysplasia requires plain radiographs and either MRI or CT scan (or both) to properly measure coverage and version.
Isolated arthroscopy should not be used to treat structural instability observed in moderate or severe dysplasia.
In properly selected patients with transitional acetabular coverage, or borderline dysplasia, good outcomes can be achieved at short- and mid-term follow-up.PAO and hip arthroscopy can be used together, either simultaneous or staged, to accurately correct both dysplasia and FAI syndrome.
In nonarthritic individuals, PAO alters the natural history of dysplasia and reduces the risk of hip arthritis and subsequent THA.文献出处:Joshua D Harris, Brian D Lewis, Kwan J Park. Hip Dysplasia. Review Clin Sports Med. 2021 Apr;40(2):271-288.
本文是陶可版权所有,未经授权请勿转载。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论