 三甲
三甲
髋关节发育不良:PAO髋臼周围截骨术后髋关节是如何发展变化的?(不同严重程度的发育不良髋关节在PAO
髋关节发育不良:PAO髋臼周围截骨术后髋关节是如何发展变化的?(不同严重程度的发育不良髋关节在PAO截骨术后能有效保髋多少年?)
作者:Cody C Wyles, Juan S Vargas, Mark J Heidenreich, Kristin C Mara, Christopher L Peters, John C Clohisy, Robert T Trousdale, Rafael J Sierra.
作者单位: Department of Orthopedic Surgery (C.C.W., J.S.V., M.J.H., R.T.T., and R.J.S.) and Division of Biomedical Statistics and Informatics (K.C.M.), Mayo Clinic, Rochester, Minnesota.
译者:陶可(北京大学人民医院骨关节科)
摘要
背景:髋臼周围截骨术(PAO)是骨骼成熟患者中症状性髋臼发育不良或发育性髋关节发育不良(DDH)的最常见治疗方法。这项多中心队列研究的目的是描绘髋臼周围截骨术(PAO)后髋关节发育不良的长期放射学自然史。
方法:我们评估了1996年至2012年在美国3个学术机构接受髋臼周围截骨术(PAO)的所有患者。纳入标准是DDH的髋臼周围截骨术(PAO)并至少进行5年的影像学随访。排除标准为单纯髋臼后倾、神经源性发育不良、Legg-Calvé-Perthes病以及既往髋关节手术(包括截骨术和关节镜检查)的髋臼周围截骨术(PAO)。共有288名患者,其中83%是女性;平均年龄和体重指数(BMI)分别为29岁和25 kg/m。平均临床和放射学随访时间为9.2年(范围为5.0至21.1年)。对每张术前和术后髋关节X线片进行评估,根据Tönnis分类确定骨关节炎的程度。通过多状态建模对生存率进行分析,从而能够通过Tönnis等级评估进展,而不仅仅是像Kaplan-Meier技术那样的个体转变。
结果:截至最终随访时,144名患者(50%)进展至少1 Tönnis 级,其中42名患者(14.6%)接受全髋关节置换术。髋臼周围截骨术(PAO)后每个Tönnis等级的平均存留年数为:Tönnis 1级为19年,Tönnis 2级为8年,Tönnis 3级为4年。在初始Tönnis较高的基础上,进展为全髋关节置换术的可能性显着增加(p < 0.001)。最显着的差异发生在Tönnis 0级或1级与Tönnis 2级之间;对于Tönnis 1级,5年和10年进展为全髋关节置换术的概率分别为2% 和11%,而Tönnis 2级分别为23%和53%。
结论:髋臼周围截骨术(PAO)有效地改变了DDH的自然史。现在可以使用基于Tönnis分级的精确放射学进展来确定自然髋关节的预后。重要的是,这项研究表明,与Tönnis 0级或1级骨关节炎患者相比,术前Tönnis 2级骨关节炎患者在髋臼周围截骨术(PAO)后10年内进展到全髋关节置换术的几率明显增加。

中青年女性,髋臼周围截骨术(PAO)术前(左图)及术后(右图,已取内固定螺钉)的双髋关节X线片
表I入组队列的患者特征
在每个参与地点获得当地机构审查委员会批准后,我们评估了1996年至2012年在3个学术机构接受髋臼周围截骨术(PAO)的所有患者,包括梅奥诊所(明尼苏达州罗彻斯特)、华盛顿大学(密苏里州圣路易斯)和犹他州大学(犹他州盐湖城)。纳入标准为因髋关节发育不良(DDH)或髋关节发育不良(DDH)同时伴有髋臼后倾而行髋臼周围截骨术(PAO),且至少进行5年影像学随访。排除标准为包括因单纯髋臼后倾、神经源性发育不良、Legg-Calv´e-Perthes病而行髋臼周围截骨术(PAO),以及任何先前的髋关节手术,包括关节镜检查和儿童截骨术。最终队列中有288名患者,其中139名来自梅奥诊所,119名来自华盛顿大学,30名来自犹他大学。总体而言,83%的患者为女性,平均年龄为29岁,平均体重指数(BMI)为25 kg/m2(表I)。平均临床和影像学随访时间为9.2年(范围为5.0至21.1年)。
137例患者在髋臼周围截骨术(PAO)时进行了同期其他手术,包括88例骨软骨成形术、31例盂唇清理术、19例盂唇修复术、11例股骨截骨术和1例转子上移术。46例患者在髋臼周围截骨术(PAO)后进行了其他手术,包括38例内固定物移除、6例髋关节镜探查、4例冲洗和清创、3例盂唇修复、1例血肿清除和1例腰肌腱松解。
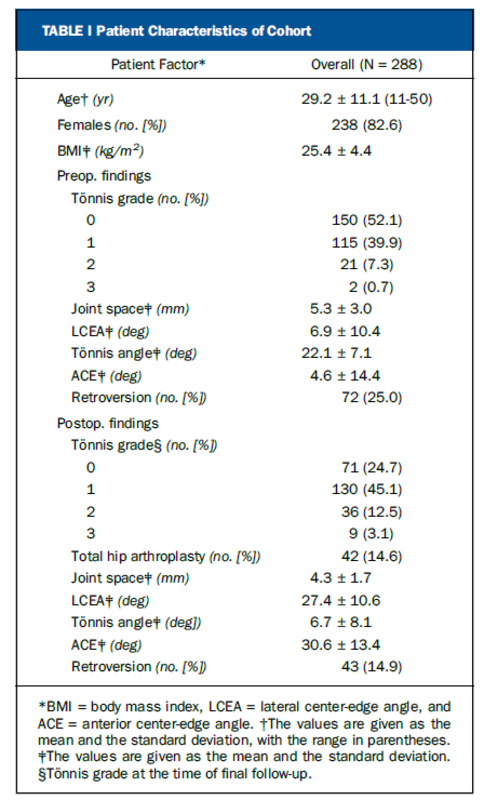
每张可用的术前和术后骨盆或髋关节前后位X线片均由2名评审员独立评估,根据Tönnis分类(0至3级)确定骨关节炎的程度。当评审者评估X线片上的Tönnis等级时,根据先前描述的分类系统标准,将患者分配到可能的最高等级。
评估人员采用以下标准:
Tönnis 0级表示不存在退行性变化;
Tönnis 1级(轻度),关节间隙轻度变窄,硬化区扩大,表现为轻度硬化,边缘有小骨赘;
Tönnis 2级(中度),关节间隙中度变窄,股骨头或髋臼中度硬化,股骨头或髋臼内存在软骨下小的骨囊肿,股骨头球形度中度丧失;
Tönnis 3级(重度),关节间隙严重变窄(<1 mm)或关节间隙闭塞,股骨头或髋臼上有大软骨下骨囊肿的证据,股骨头严重失去球形度,以及晚期骨坏死。
对每张放射学照片的评估对于通过多状态建模进行生存分析至关重要。与Kaplan-Meier技术相比,该方法结合了所有单独的放射学照相数据点来定义疾病进展,精度更高。分析中总共纳入了288名患者的2,024张X线片,每位患者中位数为7张X线片(范围为2至17张X线片)。除了Tönnis等级评估之外,术前和术后还评估了骨盆前后位以及髋关节前后位和侧位X线片,以确定如前所述的以下参数:最小关节间隙(以毫米为单位)、侧向中心边缘角 (LCEA)、Tönnis角、前中心 -边缘角(ACE)和髋臼后倾(表I)。将多状态模型确定的疾病进展与历史对照患者队列进行比较,这些患者要么患有DDH,但未接受保髋手术,要么具有正常形态的髋关节(由LCEA定义为25°至40°和Tönnis角0°至10°)。这些历史对照采用相同的统计技术进行评估,并跟踪长达35年。
*BMI = 体重指数,LCEA = 外侧中心边缘角,ACE = 前方中心边缘角。†数值以平均值和标准差形式给出,范围在括号内。‡数值以平均值和标准差的形式给出。§最终随访时的Tönnis 等级。
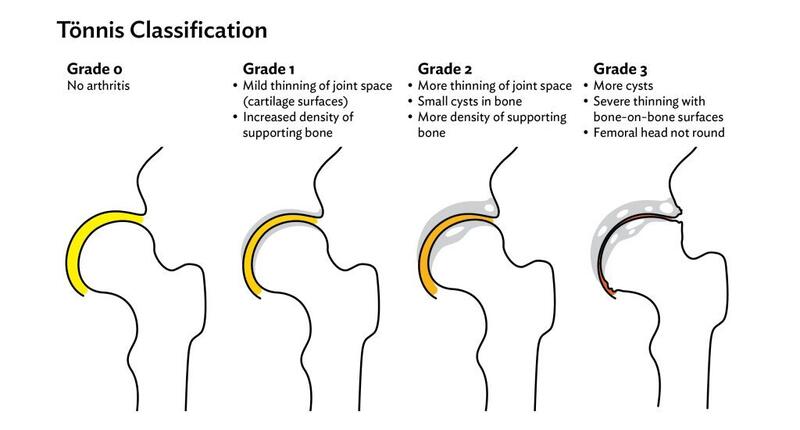
图1 研究中所有288名患者的Tönnis分级。最终随访时向各种Tönnis等级或全髋关节置换术(THA)的过渡用箭头显示。
在最终随访时{9.2年(范围为5.0至21.1年)},144名患者(50%)进展至少1个Tönnis级,其中42名患者(14.6%)接受全髋关节置换术(图1)。
具体如下:
术前,150个Tönnis 0级髋中,有76 (50.67%)髋进展到Tönnis 1级髋,有2 (1.33%)髋进展到Tönnis 2级髋,有0 (0.00%)髋进展到Tönnis 3级髋,有1 (0.67%)髋进展到全髋关节置换术(THA);
191个Tönnis 1级髋中,有52 (27.23%)髋进展到Tönnis 2级髋,有5 (2.62%)髋进展到Tönnis 3级髋,有4 (2.09%)髋进展到全髋关节置换术(THA);
75个Tönnis 2级髋中,有25 (33.33%)髋进展到Tönnis 3级髋,有14 (18.67%)髋进展到全髋关节置换术(THA);
32个Tönnis 3级髋中,有23 (71.88%)髋进展到全髋关节置换术(THA)。
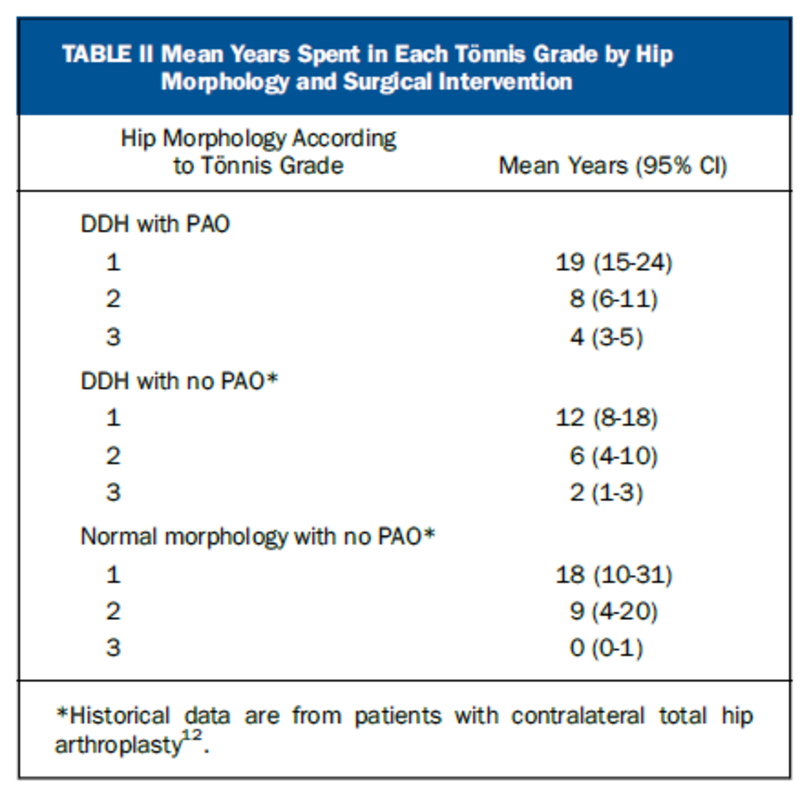
表II 根据髋关节形态学和手术干预划分的在每个Tönnis等级中停留的平均年数
髋臼周围截骨术(PAO)后每个Tönnis等级的平均年数非常接近具有正常髋关节形态的历史队列。然而,历史队列中未经治疗的髋关节发育不良(DDH)患者比形态正常的患者和当前研究中接受髋臼周围截骨术(PAO)的患者髋关节骨关节炎(OA)进展更快(表II)。
对于通过髋臼周围截骨术(PAO)的髋关节发育不良(DDH)患者,在每个Tönnis等级中停留的平均年数(近似理解为:保髋术后髋关节成功存留年数)为:Tönnis 1级为19年,Tönnis 2级为8年,Tönnis 3级为4年;
对于患有髋关节发育不良(DDH)而未接受髋臼周围截骨术(PAO)的患者,Tönnis 1级髋关节存活12年,Tönnis 2级髋关节存活6年,Tönnis 3级髋关节存活2年;
对于(股骨头)形态正常的髋关节发育不良(DDH)且未接受髋臼周围截骨术(PAO)的患者,分别为18、9和0年(表II)。
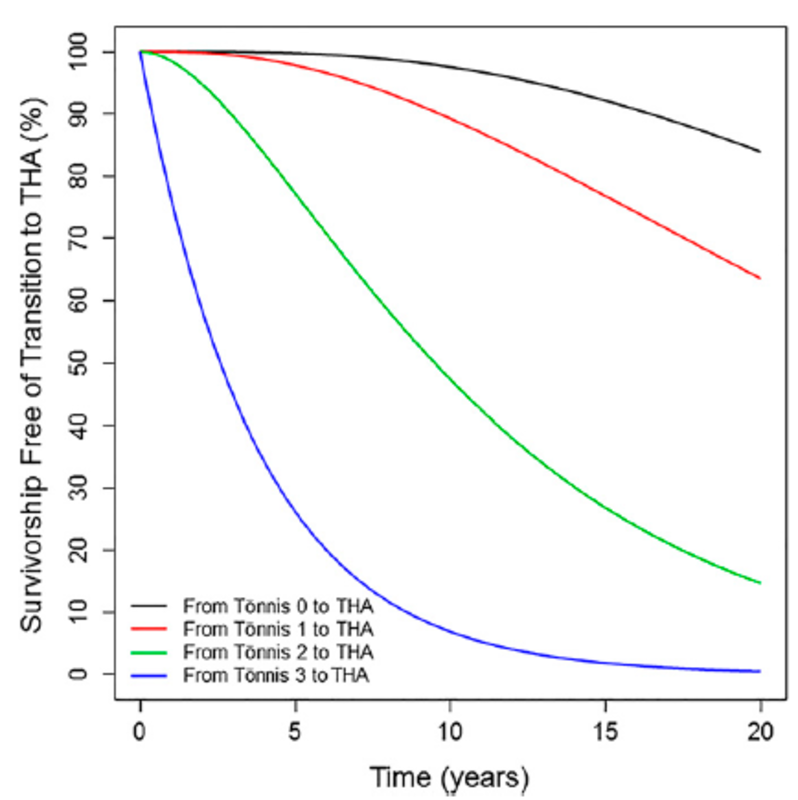
图2 多状态建模分析显示基于任何给定时间点的Tönnis等级的无全髋关节置换术(THA)的存活率。因此,当患者进展到更严重的Tönnis等级时,他们会假定指示曲线所归因的自然历史是从时间零开始。
髋臼周围截骨术(PAO)手术前Tönnis分级较高,进展为全髋关节置换术的可能性显着增加(p < 0.001)(图2)。
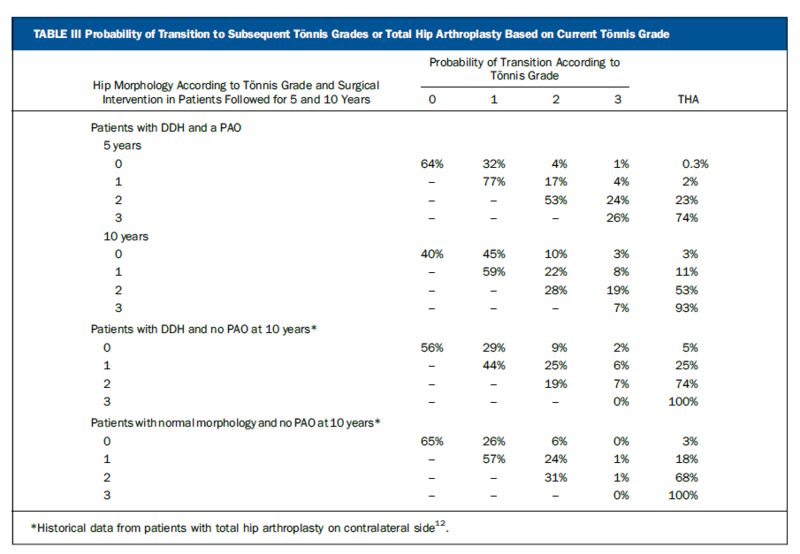
表III 基于当前Tönnis等级进展到严重Tönnis等级或全髋关节置换术的概率。
自然史最显着的差异发生在髋臼周围截骨术(PAO)时Tönnis 0级或1级患者与Tönnis 2级患者之间。
对于Tönnis 1级患者,5年和10年进展为全髋关节置换术的概率分别为2%和11%,而Tönnis 2级患者则分别为23%和53%(p < 0.001)(表III)。
髋臼周围截骨术(PAO)后,进展率和模式与历史队列中形态正常的患者相似,但与未处理的髋关节发育不良(DDH)患者相比显着改善(所有比较p < 0.05)(表III)。
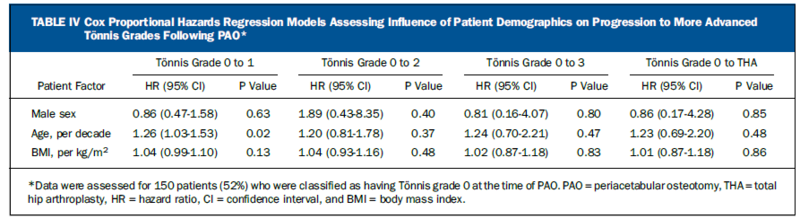
表IV Cox比例风险回归模型评估患者人口统计特征对髋臼周围截骨术(PAO)后进展至严重Tönnis等级的影响
在髋关节发育不良(DDH)组中,根据形态学和/或手术干预,髋臼周围截骨术(PAO)10年后Tönnis 1级或2级患者进展为全髋关节置换术的概率:Tönnis 1级患者为11%,Tönnis 2级患者为53%;
没有髋臼周围截骨术(PAO)的髋关节发育不良(DDH)组中:Tönnis 1级患者进展为全髋关节置换术为25%,Tönnis 2级患者进展为全髋关节置换术为74%;
在没有髋臼周围截骨术(PAO)的(股骨头)形态正常组中,这一比例为18%和68%(表III)。Cox比例风险回归模型表明,年龄、性别或BMI与髋臼周围截骨术(PAO)后进展至更严重Tönnis阶段之间没有显着的总体关系(表IV)。
Natural History of the Dysplastic Hip Following Modern Periacetabular Osteotomy.
Abstract
Background: Periacetabular osteotomy (PAO) is the most common treatment for symptomatic acetabular dysplasia, or developmental dysplasia of the hip (DDH), in skeletally mature patients. The purpose of this multicenter cohort study was to delineate the long-term radiographic natural history of the dysplastic hip following PAO.
Methods: We evaluated all patients undergoing PAO from 1996 to 2012 at 3 academic institutions in the United States. Inclusion criteria were PAO for DDH with a minimum 5-year radiographic follow-up. Exclusion criteria were PAO for isolated acetabular retroversion, neurogenic dysplasia, Legg-Calvé-Perthes disease, and prior hip surgery including osteotomies and arthroscopy. There were 288 patients, 83% of whom were women; the mean age and body mass index (BMI) were 29 years and 25 kg/m, respectively. The mean clinical and radiographic follow-up was 9.2 years (range, 5.0 to 21.1 years). Every preoperative and postoperative hip radiograph was assessed to determine the degree of osteoarthritis according to the Tönnis classification. Survivorship was analyzed by multistate modeling, enabling assessment of progression through the Tönnis grades rather than just individual transitions as with Kaplan-Meier techniques.
Results: At the time of final follow-up, 144 patients (50%) had progressed at least 1 Tönnis grade, with 42 patients (14.6%) undergoing total hip arthroplasty. The mean number of years spent in each Tönnis grade following PAO was 19 for Tönnis grade 1, 8 for Tönnis grade 2, and 4 for Tönnis grade 3. The probability of progression to total hip arthroplasty increased significantly on the basis of a higher initial Tönnis grade (p < 0.001). The most marked difference occurred between Tönnis grade 0 or 1 and Tönnis grade 2; for Tönnis grade 1, the probability of progression to total hip arthroplasty at 5 and 10 years was 2% and 11%, respectively, compared with 23% and 53%, respectively, for Tönnis grade 2.
Conclusions: PAO effectively alters the natural history of DDH. Precise radiographic progression based on the Tönnis grade can now be used to ascribe prognosis for the native hip. Importantly, this investigation demonstrates a stark increase in progression to total hip arthroplasty within 10 years of PAO for patients with preoperative Tönnis grade-2 osteoarthritis compared with those with Tönnis grade-0 or 1 osteoarthritis.
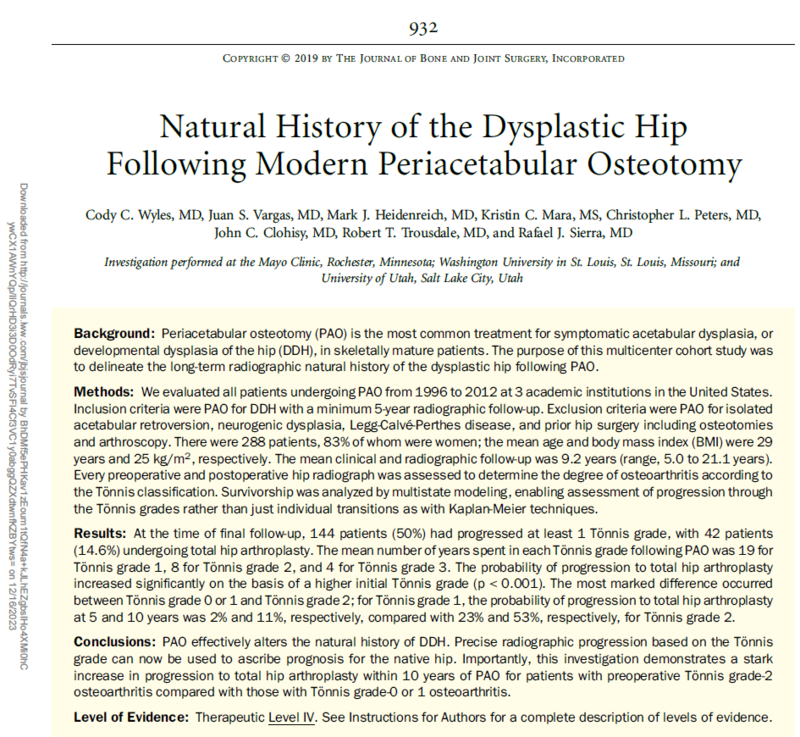
TABLE I Patient Characteristics of Cohort
Following local institutional review board approval at each participating site, we evaluated all patients undergoing PAO, from 1996 to 2012, at 3 academic institutions including the Mayo Clinic (Rochester, Minnesota), Washington University (St. Louis, Missouri), and the University of Utah (Salt Lake City, Utah). Inclusion criteria were PAO for DDH or for DDH and concomitant acetabular retroversion with a minimum 5-year radiographic follow-up. Exclusion criteria were PAO for isolated acetabular retroversion, neurogenic dysplasia, Legg-Calv´e-Perthes disease, and any prior surgery about the hip including arthroscopy and childhood osteotomies. There were 288 patients in the final cohort, with 139 from the Mayo Clinic, 119 from Washington University, and 30 from the University of Utah. Overall, 83% of the patients were women, the mean age was 29 years, and the mean body mass index (BMI) was 25 kg/m2 (Table I). The mean clinical and radiographic followup was 9.2 years (range, 5.0 to 21.1 years). Concomitant procedures at the time of PAO were performed in 137 patients and included 88 osteochondroplasties, 31 labral debridements, 19 labral repairs, 11 femoral osteotomies, and 1 trochanteric advancement. Additional procedures were performed following PAO in 46 patients and included 38 hardware removals, 6 arthroscopic explorations, 4 irrigation and debridements, 3 labral repairs, 1 hematoma evacuation, and 1 psoas tendon release.
Every available preoperative and postoperative anteroposterior radiograph of the pelvis or hip was independently assessed by 2 reviewers to determine the degree of osteoarthritis according to the Tönnis classification (grade 0 to 3). When the reviewers assessed for Tönnis grades on radiographs, patients were assigned to the highest grade possible on the basis of previously described criteria for the classification system. The following criteria were applied by the assessors: Tönnis grade 0 indicated the absence of degenerative changes; Tönnis grade 1 (mild), mild joint-space narrowing, mild sclerosis evidenced by widening of the sclerotic zone, and small marginal osteophytes; Tönnis grade 2 (moderate), moderate joint-space narrowing, moderate sclerosis of the femoral head or acetabulum, presence of small subchondral cysts within the femoral head or acetabulum, and moderate loss of femoral head sphericity; and Tönnis grade 3 (severe), severe joint-space narrowing (<1 mm) or obliteration of the joint space, evidence of large subchondral cysts on the femoral head or acetabulum, severe loss of sphericity of the femoral head, and advanced osteonecrosis. Evaluation of every radiograph was essential to enable survivorship analysis by multistate modeling. This method incorporates all individual radiographic data points for definition of disease progression with enhanced precision compared with Kaplan-Meier techniques. A total of 2,024 radiographs of the 288 patients were included in the analysis, with a median of 7 radiographs (range, 2 to 17 radiographs) per patient. In addition to Tönnis grade evaluation, anteroposterior pelvic and anteroposterior and lateral radiographs of the hip were assessed both preoperatively and postoperatively to determine the following parameters as previously described: minimum joint space in millimeters, lateral centeredge angle (LCEA), Tönnis angle, anterior center-edge angle (ACE), and acetabular retroversion (Table I)14. Progression of disease as determined by multistate modeling was compared with a historical control cohort of patients who either had DDH and did not undergo hip preservation surgery or had a hip with normal morphology as defined by an LCEA between 25° and 40° and a Tönnis angle of 0° to 10°. These historical controls were evaluated by the same statistical techniques and were followed for up to 35 years.
*BMI = body mass index, LCEA = lateral center-edge angle, and ACE = anterior center-edge angle. †The values are given as the mean and the standard deviation, with the range in parentheses. ‡The values are given as the mean and the standard deviation. §Tönnis grade at the time of final follow-up.
Fig. 1 The Tönnis grade of all 288 patients in the study. Transitions to various Tönnis grades or total hip arthroplasty (THA) at the time of final follow-up are shown with arrows.
At the time of final follow-up, 144 patients (50%) had progression of least 1 Tönnis grade, with 42 patients (14.6%) undergoing total hip arthroplasty (Fig. 1).
TABLE II Mean Years Spent in Each Tönnis Grade by Hip Morphology and Surgical Intervention
The mean number of years spent in each Tönnis grade following PAO closely approximated a historical cohort with normal hip morphology12. However, patients with unmanaged DDH from the historical cohort hadmore rapid progression than patients who had normal morphology and patients from the current study who underwent PAO (Table II). The mean number of years spent in each Tönnis grade by morphology and/or surgical intervention was 19 years in Tönnis grade 1, 8 years in Tönnis grade 2, and 4 years in Tönnis grade 3 for patients with DDH who had PAO; 12, 6, and 2 years, respectively, for patients with DDH and no PAO; and 18, 9, and 0 years, respectively, for patients with normal morphology and no PAO (Table II).
Fig. 2 Multistate modeling analysis demonstrating survivorship free of total hip arthroplasty (THA) based on the Tönnis grade at any given point in time. Thus, the moment a patient transitions to a more advanced Tönnis grade, they assume the natural history ascribed by the indicated curve, beginning at time zero.
The probability of progression to total hip arthroplasty increased significantly on the basis of a higher Tönnis grade at the time of PAO (p < 0.001) (Fig. 2).
TABLE III Probability of Transition to Subsequent Tönnis Grades or Total Hip Arthroplasty Based on Current Tönnis Grade.
The most marked difference in natural history occurred between patients who had Tönnis grade 0 or 1 and those who had Tönnis grade 2 at the time of PAO. For patients with Tönnis grade 1, the probability of progression to total hip arthroplasty at 5 and 10 years was 2% and 11%, respectively, compared with 23% and 53% for patients with Tönnis grade 2 (p < 0.001) (Table III). Following PAO, the rate and pattern of progression approximated those for patients with normal morphology from the historical cohort but were significantly improved compared with patients with unmanaged DDH (p < 0.05 for all comparisons) (Table III).
TABLE IV Cox Proportional Hazards Regression Models Assessing Influence of Patient Demographics on Progression to More Advanced Tönnis Grades Following PAO*
The 10-year probability of patients with Tönnis grade 1 or 2 progressing to total hip arthroplasty according to morphology and/or surgical intervention was 11% for patients with Tönnis grade 1 and 53% for those with Tönnis grade 2 in the group who had DDH with PAO; 25% and 74%, respectively, in the group with DDH without PAO; and 18% and 68% in the group with normal morphology without PAO (Table III). Cox proportional hazards regression models demonstrated no significant overall relationship of age, sex, or BMI with progression to more advanced Tönnis stages following PAO (Table IV).
文献出处:Cody C Wyles, Juan S Vargas, Mark J Heidenreich, Kristin C Mara, Christopher L Peters, John C Clohisy, Robert T Trousdale, Rafael J Sierra. Natural History of the Dysplastic Hip Following Modern Periacetabular Osteotomy. J Bone Joint Surg Am. 2019 May 15;101(10):932-938.doi: 10.2106/JBJS.18.00983.
本文是陶可版权所有,未经授权请勿转载。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论