
膝关节冠状面对线CPAK分类系统_不是所有的膝关节、全膝关节置换都是一样的(2024)
膝关节冠状面对线CPAK分类系统_不是所有的膝关节、全膝关节置换都是一样的(2024)Not all knees are the same
MacDessi S J, van de Graaf V A, Wood J A, Griffiths-Jones W, Bellemans J, Chen D B. Not all knees are the same[J]. Bone Joint J, 2024,106-B(6): 525-531.
转载文章的原链接1:
https://pubmed-ncbi-nlm-nih-gov-443.vpnm.ccmu.edu.cn/38821506/
转载文章的原链接2:
https://boneandjoint.org.uk/Article/10.1302/0301-620X.106B6.BJJ-2023-1292.R1
Abstract
The aim of mechanical alignment in total knee arthroplasty is to align all knees into a fixed neutral position, even though not all knees are the same. As a result, mechanical alignment often alters a patient’s constitutional alignment and joint line obliquity, resulting in soft-tissue imbalance. This annotation provides an overview of how the Coronal Plane Alignment of the Knee (CPAK) classification can be used to predict imbalance with mechanical alignment, and then offers practical guidance for bone balancing, minimizing the need for soft-tissue releases.
全膝关节置换术中的机械对线的目的是将所有膝关节对线到一个固定的中立位置,尽管并非所有膝关节都相同。因此,机械对线通常会改变患者的固有对线和关节线倾斜度,导致软组织失衡。本文概述了如何使用“膝关节冠状面对线(CPAK)”分类来预测机械对线引起的失衡,并提供了实用的指导,以平衡骨骼,减少对软组织释放的需要。
Introduction
Irrespective of the alignment strategy used when undertaking total knee arthroplasty (TKA), surgeons must contend with the fact that not all knees are the same. In mechanically aligned TKA, balancing is usually performed following completion of the bony cuts and assessment of the laxity of the soft-tissues.1 The long-standing approach for achieving balanced “gaps” has been by releasing or lengthening ligamentous and capsular structures, thereby altering their inherent physiological function.1,2 With a greater acceptance that ligaments do not contract,3 and that imbalance results from surgical alterations to the patient’s constitutional alignment,4 a more nuanced approach with “bone balancing” has been suggested.5
Bone balancing modifies the alignment by biasing bony resections towards a more constitutional orientation, thereby maintaining their function and reducing the necessity for soft-tissue releases. Bone balancing using an initial mechanical alignment plan represents one end of the spectrum of TKA alignment strategies, with unrestricted kinematic alignment at the other.6-10 Subtle changes of alignment up to 3° from a neutral mechanical axis are often enough to improve imbalance, and still considered safe for surgeons who want to maintain alignment within this more traditional window.11,12
Restoring the knee’s constitutional alignment is more likely to achieve soft-tissue balance compared with using mechanical alignment for all patients.13,14 The Coronal Plane Alignment of the Knee (CPAK) classification is a widely adopted and pragmatic system that offers a framework to understand the relationship between the native lower limb alignment and joint line obliquity (JLO) to the soft-tissue balance.14 CPAK defines nine knee phenotypes based on constitutional alignment of the knee, incorporating the arithmetic hip-knee-ankle angle (aHKA) and the joint line obliquity.
In this instructional review, we use the CPAK classification to understand why not all knees are the same in terms of imbalance when performing mechanically aligned TKA. Each CPAK type will be introduced based on its primary radiological and morphological characteristics. Alterations to constitutional alignment that result when performing mechanically aligned TKA will be presented for each CPAK type, along with the anticipated challenges with balance. For most surgeons who use mechanical alignment, and for those who have now adopted an individualized approach, understanding these concepts is important for appreciating why alignment matters.
Radiological assessment
Preoperative long leg imaging that allows for assessment of the mechanical axis is obtained
using plain radiographs with digital stitching, biplanar imaging or whole-leg CT imaging. The lateral distal femoral angle (LDFA) is measured as the lateral angle subtended by the mechanical axis of the femur and the articular line tangential to the distal femoral articular surface. The medial proximal tibial angle (MPTA) is measured as the medial angle subtended by the mechanical axis of the tibia and the articular line tangential to the proximal tibial articular surface (Figure 1). Apart from highlighting loss of joint space, short radiographs of the knee are of no value in the assessment of constitutional alignment, and therefore of the individual’s knee phenotype.15,16
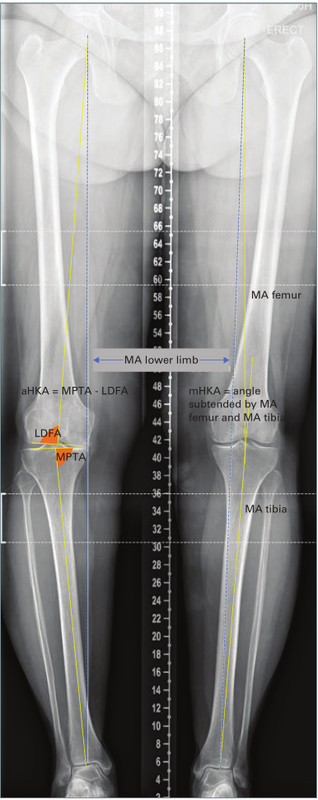
Fig. 1 Long leg standing radiographs showing the mechanical axes of the femur and tibia. The right knee shows measurement of constitutional alignment in an arthritic knee using the arithmetic hip-knee-ankle angle (aHKA) algorithm. The left normal knee shows measurement of the the mechanical hip-knee-ankle angle (mHKA). LDFA, lateral distal femoral angle; MA, mechanical axis; MPTA, medial proximal tibial angle.
The constitutional coronal alignment is calculated using the equation aHKA = MPTA – LDFA, and the constitutional joint line obliquity (JLO) using the equation JLO = MPTA + LDFA. The boundaries for constitutional alignment of the lower limb using the aHKA are varus < -2°, neutral -2° to +2° inclusive, and valgus > 2°. The boundaries for constitutional JLO are apex distal < 177°, neutral 177° to 183°, and apex proximal > 183°. The CPAK type is then determined based on these boundaries (Figure 2).
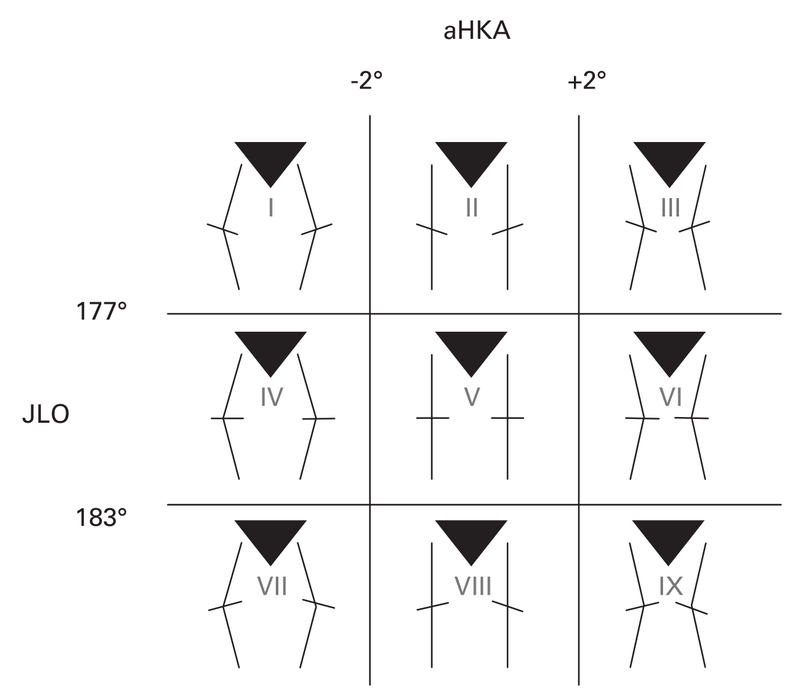
Fig. 2 The Coronal Plane Alignment of the Knee (CPAK) classification with boundaries. aHKA, arithmetic hip-knee-ankle; JLO, joint line obliquity.
Data from previous studies support the descriptions of each CPAK type discussed here. Alignment characteristics are derived from a sample of 500 knees in 250 healthy adults, aged between 20 and 27 years (Supplementary Table i);13 soft-tissue laxity data are derived from a sample of 137 knees comparing balance between different alignment strategies (Supplementary Table ii);17 and load sensor data are derived from a sample of 138 knees comparing compartmental loads between alignment strategies (Supplementary Table iii).4
In this annotation, only CPAK Types I to VI are discussed, as many authors have shown that Types VII to IX are rare in the general population.14,18-23 For the LDFA and MPTA, we characterize orientation as “neutral” if ≤ 1° from 90°; “mild” if > 1°and ≤ 2° from 90°; “moderate” if > 2° and ≤ 4° from 90°; and “significant” if > 4° from 90°. Descriptive radiological measurements and schematic phenotypic traits are presented for each CPAK type and for changes to JLO. Alterations in constitutional alignment, native femoral joint line anatomy, lateral femoral column length, and their sequelae are summarized in Table I.
Table I. The implications of mechanical alignment based on Coronal Plane Alignment of the Knee type.
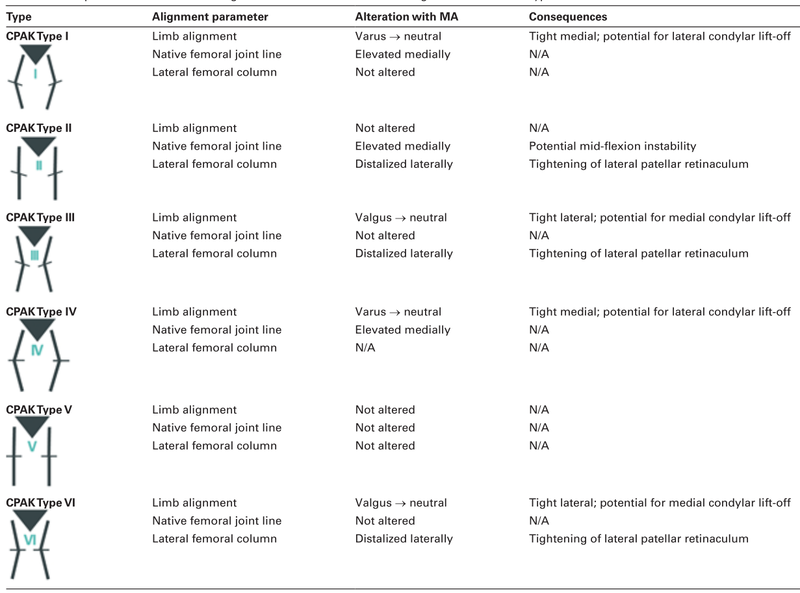
CPAK, Coronal Plane Alignment of the Knee; MA, mechanical alignment; N/A, not applicable.
CPAK Type I
The knees in 133 of the sample of healthy individuals (26.6%) were CPAK Type I. This is the most prevalent phenotype in Asian and Indian patients undergoing TKA, and is the most common varus phenotype globally.18,19,23 This type is characterized by significant proximal tibial varus and mild distal femoral valgus, resulting in a varus aHKA and an apex distal JLO. The implications for mechanical alignment are shown in Figure 3a.
Mehanical alignment with CPAK Type I knees results in considerable tightness of the MCL due to the shift in aHKA from varus to neutral. As the magnitude of change increases, so does the likelihood of lateral condylar lift-off, a signal of major imbalance. The MCL is tight in both extension and flexion. Commonly, surgeons partially or completely release the MCL in an attempt to achieve balance, but secondary incompetence of the MCL may result from releasing this critical structure. Alteration of constitutional varus to neutral will increase the length of the leg, and increase the need for a thicker polyethylene insert to compensate for the artificial increase in medial gap height.24 As the primary characteristic of Type I is tibial varus, a varus tibial recut with mechanical alignment may be required to achieve balance in both extension and flexion.
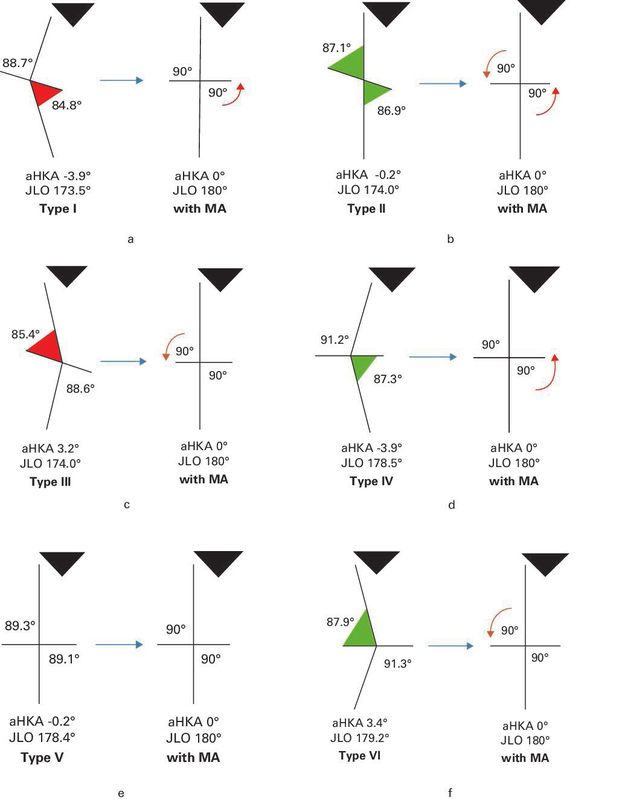
Fig. 3 Illustration of soft-tissue imbalance in Coronal Plane Alignment of the Knee (CPAK) Types I to VI, showing how mechanical alignment (MA) alters constitutional alignment and joint line obliquity.
a) MA with CPAK Type I. The red wedge highlights significant tibial varus, and the red arrow indicates elevation of the medial joint line.
b) MA with CPAK Type II. The green wedges highlight moderate femoral valgus and moderate tibial varus. The red arrow indicates elevation of the medial joint line, and the orange arrow indicates distalization of the lateral femoral column.
c) MA with CPAK Type III. The red wedges highlights significant femoral valgus, and the orange arrow indicates distalization of the lateral femoral column.
d) MA with CPAK Type IV. The green wedge indicates moderate tibial varus. The red arrow highlights elevation of the medial joint line.
e) MA with CPAK Type V.
f) MA with CPAK Type VI. The green wedge highlights moderate femoral valgus and the orange arrow indicates distalization of the lateral femoral column.
aHKA, arithmetic hip-knee-ankle angle; JLO, joint line obliquity.
CPAK Type II
The knees of 205 of the healthy individuals (41.0%) were CPAK Type II. This is the most common knee phenotype globally.14,22 This type is characterized by moderate proximal tibial varus and moderate distal femoral valgus, resulting in a neutral aHKA and an apex distal JLO. The implications for mechanical alignment are shown in Figure 3b.
Mechanically aligned TKA specifically addresses CPAK Type II phenotypic characteristics. As neutral constitutional alignment is maintained, soft-tissue balance in extension is usually not altered. Furthermore, by applying external rotation to the femoral component, imbalance in flexion is unlikely. The “anatomical alignment” method attempted to replicate Type II by recreating an apex distal JLO,25 but imprecise cutting guides resulted in this technique being abandoned.
The following kinematic alterations require consideration in CPAK Type II. The native femoral joint line is raised medially throughout the arc of motion, a potential cause of mid-flexion instability.26 The lateral femoral column is lengthened (distalized) in extension and flexion. It has been suggested that this may lead to increased patellofemoral retinacular tightness in flexion by lateral distal femoral prosthetic overstuffing,27 particularly in knees with very oblique joint lines such as those of ≤ 170°. The need for soft-tissue balancing with CPAK Type II is minimal.
CPAK Type III
The knees of 47 of the healthy individuals (9.4%) were CPAK Type III. This type is the most common valgus phenotype and is characterized by considerable distal femoral valgus and mild proximal tibial varus, resulting in a valgus aHKA and apex distal JLO. The implications for mechanical alignment are shown in Figure 3c.
Imbalance with mechanical alignment occurs in extension and to a lesser extent in flexion, as the aHKA is shifted from valgus to neutral. The degree of lateral tightness is dependent on two variables: the magnitude of aHKA relative to the change prescribed by mechanical alignment; and the variability in constitutional laxity of the lateral side relative to medial laxity. In many knees, increased constitutional lateral laxity, which is further increased after resection of the cruciate ligaments,28–30 can compensate for this shift in aHKA and reduce the need for lateral balancing. However, in our experience, when patients have an aHKA of ≥ 5°, soft-tissue imbalance inevitably results. As the primary characteristic of CPAK Type III is significant femoral valgus, a distal femoral valgus recut may be required to achieve balance in extension.
CPAK Type IV
The knees of 21 of the healthy individuals (4.2%) were CPAK Type IV, which is a rarer varus phenotype, characterized by moderate proximal tibial varus and mild distal femoral varus, resulting in a varus aHKA and neutral JLO. The implications for mechanical alignment are shown in Figure 3d.
As with Type I, there will be MCL tightness in CPAK Type IV with mechanically aligned TKA. However, this tightness is more prominent in extension than flexion.14 As the major anatomical characteristic in CPAK Type IV is tibial varus, a varus tibial recut may be required to restore balance in both extension and flexion, although an additional varus femoral recut can be considered.
CPAK Type V
The knees of 77 of the healthy individuals (15.4%) were CPAK Type V, which is the target in mechanically aligned TKA. This type is characterized by neutral distal femoral and neutral proximal tibial anatomy, resulting in a neutral aHKA and neutral JLO. The implications for mechanical alignment are shown in Figure 3e.
No balancing interventions are usually necessary for CPAK Type V with mechanical alignment. However, unlike CPAK Type II knees, the tibial joint line is not changed, and surgeons should evaluate whether the routine 3° external rotation of the femoral component is needed.
CPAK Type VI
The knees of 16 of the healthy individuals (3.2%) were CPAK Type VI. This type makes up approximately one-quarter of all valgus knees, and is characterized by moderate distal femoral valgus and mild proximal tibial valgus, resulting in a valgus aHKA and neutral JLO. The implications for mechanical alignment are shown in Figure 3f.
Compared with CPAK Type III, constitutional valgus is contributed to by femoral valgus and, to a lesser extent, tibial valgus. This results in a neutral joint line obliquity. Soft-tissue imbalance is most pronounced in extension.14 As the main characteristic of Type VI is femoral valgus, a valgus femoral recut may be required if there is marked lateral tightness in extension. If there remains some imbalance, or when femoral recuts are preferably avoided, a release of the posterolateral capsular (arcuate) complex, with or without the posterior band of the iliotibial band, may be considered.31
Discussion
This instructional annotation presents a method, based on constitutional alignment, for understanding and predicting the soft-tissue imbalance that often results when undertaking mechanically aligned TKA. It provides clear, alignment-driven reasoning based on deviations to common CPAK phenotypes. Imbalances are most profound in constitutional varus knees, Types I and IV. However, constitutional valgus knees, Types III and VI, also present intraoperative challenges. The ability to understand the likelihood of encountering imbalance prior to, and during, surgery is empowering. The concepts can also be used by those who use a gap-balancing approach with conventional cutting guides, as they streamline the workflow of both tibial- and femoral-based techniques.
Most importantly, not all knees are the same, and there will be much variation between individuals, even within each CPAK type. Thus, one patient with a Type II knee may have a LDFA of 88° and MPTA of 88°, another may have a LDFA of 84° and MPTA of 83°. Treating both knees with the same mechanically aligned resections is likely to bring about different kinematic results. Or, when a patient with a Type I knee with an aHKA of -3° may only require a 2° varus recut in order to obtain a balanced knee, another, also with a Type I knee, but an aHKA of -7°, is unlikely to be balanced with a small varus correction from mechanical alignment. Furthermore, CPAK is a classification system to describe phenotypes and is not granular enough to provide a comprehensive breakdown of how balancing should be executed when performing mechanically aligned TKA.
Furthermore, it is not only the constitutional alignment but also the constitutional laxity that determines the balance of a TKA. Native laxities are highly variable in both the coronal (extension and flexion) and sagittal planes.32-35 Thus, a knee can have its constitutional alignment perfectly restored, as in unrestricted kinematic alignment, but still have unbalanced gaps.17,36 Targeting balanced coronal and sagittal gaps remains a major goal in TKA and is the cornerstone of the functional alignment technique.17,36,37 However, the optimal balance, including whether rectangular or trapezoidal constitutional gaps should be the new target, remains poorly defined. Surgeons must continue to use their clinical acumen to assess each knee on its merits, applying the knowledge of outcomes determined by phenotype, to optimize alignment and balance.
Conventional cutting guides with mechanical alignment have also been reported to have precision errors of > 3° in 30% of cases,38 with half of those cases potentially deviating into more than 3° varus (15%) and half into more than 3° valgus (another 15%). For example, if a surgeon aiming for mechanical alignment using conventional instruments unintentionally alters the HKA of a knee that has 5°of constitutional varus to ≥ 4°of mechanical valgus, this could result in a profound change in alignment of 9°, the type of situation that could occur in 1 in 6 (15%) of mechanically aligned TKAs undertaken using conventional cutting guides. Severe tightness of the MCL will result in lateral condylar lift-off. The only way to correct this imbalance is to release the MCL from its tibial insertion. This will result in an increase in both medial flexion and extension gaps, the subsequent need for a thicker polyethylene insert, and a net effect of lengthening the limb.24 Correction towards a more varus phenotype is preferred to a complete release of the MCL. The inherent limitations of conventional cutting guides are that they do not allow quantification or validation of the angles of resection or the final alignment of the limb.
As we gradually shift towards more personalized operations for our patients, it is hoped that this annotation will encourage surgeons to consider each patient’s unique CPAK type. This, in part, may make the outcomes of TKA more predictable, reducing the need for soft-tissue releases while using adjustments in alignment to restore the native balance of the knee.
Take home message
- In this review, the Coronal Plane Alignment of the Knee (CPAK) classification is used to enhance our understanding of why not all knees are the same when considering soft-tissue imbalance in mechanically aligned total knee arthroplasty.
- Bone balancing interventions based on an understanding of each patient’s unique CPAK type can be used to avoid unnecessary soft-tissue releases.
- These concepts may be considered by surgeons interested in a more individualized alignment strategy, instead of a fixed mechanical alignment target for all patients.
在本综述中,采用“膝关节冠状面排列(CPAK)”分类来增强我们对在机械对线全膝关节置换术中考虑软组织失衡时为何并非所有膝关节都相同的理解。
基于对每位患者独特CPAK类型的理解,可以实施骨平衡干预措施,以避免不必要的软组织释放。
这些概念可能对有兴趣采用更个性化对齐策略的外科医生有所帮助,而不是为所有患者设定固定的机械对线目标。

本文为转载文章,如有侵权请联系作者删除。本文仅供健康科普使用,不能做为诊断、治疗的依据,请谨慎参阅





评论